Electrochemical Biosensors for Fusion Gene Detection: A Transformative Approach for Cancer Diagnostics
This article explores the convergence of electrochemical biosensing technology and fusion gene analysis for advanced cancer diagnostics.
Electrochemical Biosensors for Fusion Gene Detection: A Transformative Approach for Cancer Diagnostics
Abstract
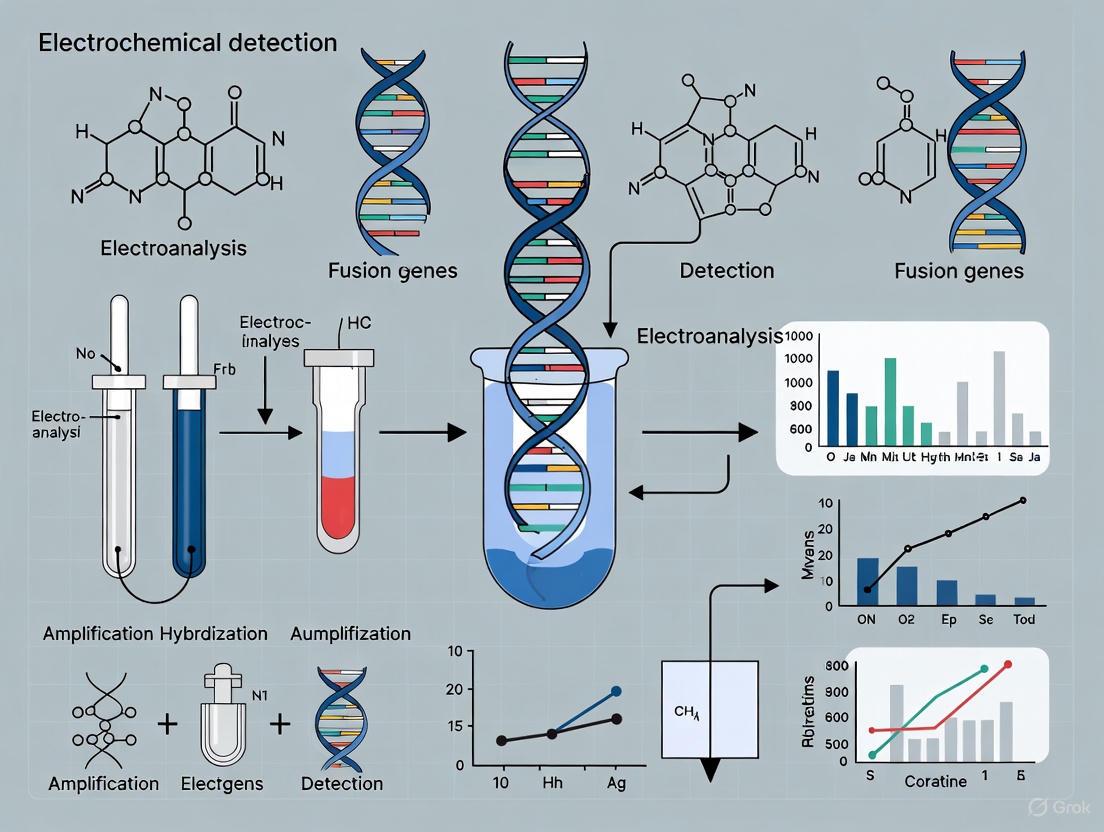
This article explores the convergence of electrochemical biosensing technology and fusion gene analysis for advanced cancer diagnostics. Fusion genes are pivotal oncogenic drivers in numerous cancers, serving as critical biomarkers for diagnosis, prognosis, and targeted therapy. While methods like FISH, PCR, and NGS are established for their detection, they often face limitations in cost, speed, and point-of-care applicability. This review details how electrochemical biosensors, enhanced by nanomaterials and microfluidics, offer a promising alternative with high sensitivity, rapid response, and potential for miniaturized, low-cost devices. We cover the foundational biology of fusion genes, the design and operational principles of electrochemical genosensors, strategies to overcome analytical and biological challenges, and a comparative analysis with traditional techniques. Aimed at researchers, scientists, and drug development professionals, this synthesis highlights the potential of electrochemical sensing to revolutionize liquid biopsy and enable routine, early cancer detection.
The Critical Role of Fusion Genes in Cancer and the Electrochemical Sensing Principle
Oncogenic gene fusions are hybrid genes resulting from chromosomal rearrangements such as translocations, inversions, deletions, or tandem duplications [1]. These fusion events can create potent driver oncogenes that play a defining role in cancer pathogenesis, making them valuable clinical biomarkers for diagnosis, prognosis, and targeted therapy selection [1] [2]. The discovery of the Philadelphia chromosome in 1960, later identified as the BCR-ABL fusion in chronic myeloid leukemia (CML), marked the first recognized fusion gene in cancer [1]. Since then, numerous clinically significant fusions have been identified across diverse cancer types, including EML4-ALK in non-small cell lung cancer (NSCLC) and NTRK fusions across multiple tumor types [1] [3].
These fusion genes typically result in constitutive activation of tyrosine kinase signaling pathways, leading to uncontrolled cell proliferation and survival [4] [3]. From a clinical perspective, fusion genes represent clonal mutations present in all cancer cells of a patient, making them ideal personal cancer targets for therapeutic intervention [5] [3]. The growing importance of detecting these biomarkers is reflected in the finding that gene fusions occur in up to 17% of all solid tumors, with certain cancer types exhibiting particularly high prevalence rates [3].
Table 1: Prevalence of Key Oncogenic Fusion Genes in Cancer
| Fusion Gene | Primary Cancer Types | Prevalence | Clinical Significance |
|---|---|---|---|
| BCR-ABL | Chronic Myeloid Leukemia (CML) | ~95% of CML [4] | Defining diagnostic marker; target for TKIs |
| EML4-ALK | Non-Small Cell Lung Cancer (NSCLC) | 2-7% of NSCLC [3] | Targeted by multiple FDA-approved inhibitors |
| NTRK Fusions | Multiple rare tumors (e.g., secretory carcinoma, infantile fibrosarcoma) | ~100% in some rare tumors [1] [4] | Paradigm for tumor-agnostic therapy |
| TMPRSS2-ERG | Prostate Cancer | ~50% of prostate cancers [1] | Most common ETS family fusion in prostate cancer |
| RET Fusions | Thyroid Cancer, NSCLC | Varies by cancer type [1] | Target for selective RET inhibitors |
Detection Methodologies for Fusion Genes
Conventional Detection Approaches
Traditional methods for fusion gene detection include fluorescence in situ hybridization (FISH), immunohistochemistry (IHC), and polymerase chain reaction (PCR)-based techniques [1]. While these methods remain valuable in clinical diagnostics, they possess inherent limitations for multiplexed analysis and novel fusion discovery [1]. FISH provides visual localization of chromosomal rearrangements but offers limited information about fusion partners and breakpoints. IHC detects protein overexpression resulting from fusion events but lacks specificity for specific fusion variants [1].
Next-Generation Sequencing Platforms
Next-generation sequencing (NGS) technologies have revolutionized fusion gene detection by enabling comprehensive analysis of multiple genes simultaneously [1] [5]. Both DNA-based and RNA-based NGS approaches are employed, with RNA sequencing particularly valuable for detecting functional fusion transcripts [1]. These technologies allow for the identification of novel fusion partners and rare rearrangement events that would be missed by targeted approaches. The economic and technical challenges of implementing NGS in routine clinical care globally remain a consideration, despite growing guideline recommendations [1].
Emerging Electrochemical Biosensing Platforms
Recent advancements in electrochemical biosensors present promising alternatives for fusion gene detection, particularly in resource-limited settings [6] [7]. These platforms offer cost-effective, rapid analysis with potential for point-of-care testing, addressing accessibility gaps in cancer diagnostics [6]. Nanoengineered electrochemical biosensors incorporate advanced materials to enhance sensitivity and specificity for detecting DNA, RNA, and protein biomarkers [6] [7].
The fundamental principle involves immobilization of specific capture probes (e.g., oligonucleotides complementary to fusion junction sequences) on electrode surfaces, with detection achieved through measurable electrical signals changes upon target binding [6]. Electrode geometry and surface chemistry are critically optimized parameters, with designs including disc-shaped and microneedle electrodes to improve electroanalytical performance [6]. The integration of nanomaterials such as graphene, carbon nanotubes, and metal nanoparticles significantly enhances signal amplification, enabling detection of low-abundance fusion transcripts [7].
Table 2: Comparison of Fusion Gene Detection Methodologies
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| FISH | Fluorescently labeled DNA probes bind to specific chromosomal regions | Established clinical validity; visual confirmation of rearrangement | Limited multiplexing; cannot identify novel partners |
| IHC | Antibody detection of overexpressed fusion proteins | Rapid; cost-effective; widely available | Indirect detection; limited specificity for fusion variants |
| RT-PCR | Amplification of fusion transcript sequences | High sensitivity; quantitative potential | Requires prior knowledge of fusion partners |
| NGS | Massive parallel sequencing of DNA or RNA | Comprehensive; discovers novel fusions; multiplexed | Higher cost; complex data analysis; technical expertise |
| Electrochemical Biosensors | Electrode-based detection of hybridization events | Rapid; low-cost; point-of-care potential; high sensitivity | Still in development for fusion genes; requires validation |
Experimental Protocols
RNA Extraction and Quality Control Protocol
Principle: High-quality RNA is essential for reliable fusion gene detection by sequencing or electrochemical biosensing platforms [1].
Reagents:
- TRIzol reagent or equivalent RNA stabilization solution
- DNase I enzyme for genomic DNA removal
- RNA quality assessment reagents (e.g., Agilent Bioanalyzer RNA kits)
- Nuclease-free water and consumables
Procedure:
- Sample Preparation: Homogenize 20-30 mg of fresh frozen tissue or cell pellet in 1 mL TRIzol reagent. For formalin-fixed paraffin-embedded (FFPE) tissue, use specialized extraction kits designed for cross-linked RNA.
- Phase Separation: Add 0.2 mL chloroform per 1 mL TRIzol, shake vigorously for 15 seconds, and incubate at room temperature for 3 minutes. Centrifuge at 12,000 × g for 15 minutes at 4°C.
- RNA Precipitation: Transfer aqueous phase to new tube, mix with 0.5 mL isopropyl alcohol, and incubate at room temperature for 10 minutes. Centrifuge at 12,000 × g for 10 minutes at 4°C.
- RNA Wash: Wash pellet with 75% ethanol, vortex, and centrifuge at 7,500 × g for 5 minutes at 4°C.
- DNase Treatment: Resuspend RNA pellet in nuclease-free water and treat with DNase I following manufacturer's protocol to remove genomic DNA contamination.
- Quality Control: Assess RNA integrity number (RIN) using Bioanalyzer (target RIN >7.0 for NGS) or similar system. Verify concentration by spectrophotometry (A260/A280 ratio ~2.0).
Technical Notes: For electrochemical sensing applications, additional fragmentation may be required to optimize target accessibility. Always include positive and negative control samples in each extraction batch.
Electrochemical Detection of EML4-ALK Fusion Transcript
Principle: This protocol details specific detection of the EML4-ALK fusion transcript using a nanomaterial-enhanced electrochemical biosensor [6] [7].
Reagents:
- Gold electrode array (2 mm diameter working electrodes)
- Thiolated capture probe: 5'-HS-(CH2)6-XXXXX-3' (complementary to EML4-ALK fusion junction)
- Graphene oxide-gold nanoparticle nanocomposite
- Methylene blue redox indicator
- Phosphate buffer saline (PBS, pH 7.4) with 0.1 M NaCl
- Target EML4-ALK fusion transcript standards
Procedure:
- Electrode Modification: Polish gold electrodes with 0.3 and 0.05 μm alumina slurry, rinse with deionized water, and electrochemically clean in 0.5 M H2SO4 by cyclic voltammetry scanning from 0 to 1.5 V until stable voltammogram is obtained.
- Nanocomposite Preparation: Synthesize graphene oxide-gold nanoparticle nanocomposite by chemical reduction of HAuCl4 on graphene oxide sheets. Characterize by TEM and UV-Vis spectroscopy.
- Probe Immobilization: Incubate electrodes with 1 μM thiolated capture probe in PBS at 4°C for 16 hours. Backfill with 1 mM 6-mercapto-1-hexanol for 1 hour to block nonspecific binding sites.
- Hybridization: Apply 10 μL sample containing target RNA to electrode surface. Incubate at 42°C for 30 minutes in humidified chamber. Wash with PBS to remove unbound material.
- Electrochemical Measurement: Perform differential pulse voltammetry from -0.2 to -0.5 V in PBS containing 50 μM methylene blue. Measure reduction current at -0.35 V.
- Data Analysis: Quantify fusion transcript concentration based on calibration curve generated with known standards. Normalize signals to internal control probes.
Technical Notes: Optimal capture probe design requires precise alignment with the specific EML4-ALK variant breakpoint. Include mismatch controls to verify specificity. The assay demonstrates detection limits approaching 1 fM for synthetic targets [6].
Signaling Pathways and Molecular Mechanisms
Oncogenic fusion proteins drive tumorigenesis through constitutive activation of critical signaling pathways, particularly those involving tyrosine kinases [1] [4]. The molecular structure of kinase fusion proteins typically places the kinase domain under the control of strong promoter elements or fuses it to dimerization domains, resulting in ligand-independent activation [4] [3].
The BCR-ABL fusion protein exhibits constitutive ABL tyrosine kinase activity, leading to persistent activation of downstream pathways including RAS/MAPK, JAK/STAT, and PI3K/AKT, which collectively promote proliferation and suppress apoptosis [1]. Similarly, EML4-ALK fusions result in oligomerization through the EML4 portion, activating the ALK kinase domain and its downstream signaling cascades including RAS/ERK, STAT3, and mTOR pathways [4] [3].
NTRK fusions involve the 3' kinase domain of NTRK genes (NTRK1, NTRK2, or NTRK3) fused to various 5' partner genes, leading to ligand-independent dimerization and constitutive activation of MAPK, PI3K/AKT, and PLCγ pathways [1] [4]. These signaling events promote cell survival, proliferation, and differentiation in TRK-expressing neurons, but drive oncogenesis when activated inappropriately in other cell types.
Therapeutic Targeting and Clinical Applications
Approved Targeted Therapies
The constitutive kinase activation resulting from oncogenic fusions creates therapeutic vulnerabilities that can be exploited with targeted inhibitors [1] [3]. Tyrosine kinase inhibitors (TKIs) have demonstrated remarkable efficacy in fusion-driven cancers, with several agents receiving FDA approval for specific fusion indications [3]. These inhibitors are classified by their mechanism of action: Type I and II inhibitors compete with ATP binding in active and inactive kinase conformations, respectively, while Type III and IV are allosteric inhibitors, and Type V are bivalent inhibitors targeting two distinct regions [3].
For ALK fusion-positive NSCLC, multiple generations of inhibitors have been developed. Crizotinib, a first-generation ALK inhibitor, showed superior response rates compared to chemotherapy (ORR 74% vs. 45% in treatment-naïve patients) but faced limitations with acquired resistance [3]. Second-generation inhibitors including ceritinib, alectinib, and brigatinib offer improved potency and central nervous system penetration, with alectinib demonstrating significantly prolonged progression-free survival compared to crizotinib (median PFS not reached vs. 10.2 months) [3]. Lorlatinib, a third-generation inhibitor, maintains efficacy against resistant mutations and showed dramatic improvement in PFS (HR: 0.28) in the CROWN trial [3].
The tissue-agnostic approval of TRK inhibitors (larotrectinib and entrectinib) for NTRK fusion-positive cancers represents a paradigm shift in precision oncology, demonstrating that molecular alterations can transcend histologic classifications in guiding therapy [1] [4].
Research Reagent Solutions
Table 3: Essential Research Reagents for Fusion Gene Investigation
| Reagent Category | Specific Examples | Application & Function | Technical Notes |
|---|---|---|---|
| Cell Line Models | Ba/F3 cells expressing EML4-ALK variants; KM-12 (COL1A1-PDGFB); CUTO-3.29 (EML4-ALK) [4] | Functional validation of fusion oncogenicity; drug screening | Verify fusion status regularly; use low passages |
| Antibodies | Phospho-ALK (Tyr1604); Pan-TRK (EPR17341); BCR (C-1); c-ABL (24-11) | Detection of fusion proteins and activation status; Western blot, IHC | Validate for specific applications; check species reactivity |
| qPCR Assays | Fusion-specific TaqMan assays; SYBR Green with breakpoint-specific primers | Quantitative fusion transcript detection; minimal residual disease monitoring | Design primers spanning breakpoint junctions |
| CRISPR Tools | Guide RNAs targeting fusion junctions; Cas9 expression vectors | Functional knockout of fusion genes; mechanistic studies | Verify specificity to avoid wild-type gene targeting |
| Kinase Assays | ADP-Glo Kinase Assay System; mobility shift assays | Biochemical assessment of fusion kinase activity and inhibition | Include both wild-type and fusion kinases for comparison |
| Structural Biology | KinaseFusionDB database; predicted 3D structures [4] | In silico analysis of fusion protein structure; drug binding predictions | Use for inhibitor design and resistance mechanism studies |
Experimental Workflow for Fusion Gene Analysis
A comprehensive approach to fusion gene analysis integrates multiple methodological platforms to overcome the limitations of individual techniques [1] [6]. The following workflow diagram illustrates a integrated protocol for fusion gene detection and validation:
This integrated workflow begins with appropriate sample collection and nucleic acid extraction, followed by rigorous quality control assessment [1]. Next-generation sequencing serves as a discovery platform to identify known and novel fusion events [1] [5]. Electrochemical biosensors provide rapid, cost-effective confirmation of specific fusion targets, particularly valuable for repeated monitoring or resource-limited settings [6] [7]. Orthogonal validation using established methods (FISH, RT-PCR) ensures result reliability before proceeding to functional characterization in model systems [1]. Finally, clinical correlation links molecular findings with patient outcomes and therapeutic responses.
The application of this workflow enables comprehensive fusion gene analysis while balancing diagnostic accuracy with practical considerations of cost, throughput, and technical feasibility. This approach supports both clinical diagnostics and research investigations into novel fusion events and their biological significance.
Gene fusions are hybrid genes formed when two previously independent genes combine, often as a result of chromosomal rearrangements such as translocations, deletions, or inversions [8]. These events can produce chimeric proteins with novel functions or alter the regulation of gene expression, playing a significant role in cellular physiology and disease. In cancer, gene fusions are recognized as powerful driver mutations, contributing to an estimated 20% of global cancer morbidity [9]. The initial discovery of the BCR-ABL1 fusion gene in chronic myeloid leukemia, resulting from a translocation between chromosomes 9 and 22 (the Philadelphia chromosome), established the foundational model for understanding the oncogenic potential of fusion genes [8]. Subsequent research has identified over 10,000 gene fusions, with their prevalence varying widely across cancer types [9]. This document details the molecular mechanisms behind gene fusion formation and provides standardized protocols for their detection, with particular emphasis on applications in developing electrochemical biosensors for cancer diagnostics.
Fundamental Mechanisms of Formation
Chromosomal Translocations
Chromosomal translocations occur when segments from two different chromosomes break and exchange places. Reciprocal translocations, involving a two-way exchange of genetic material, are a primary mechanism for gene fusion [10]. If this exchange does not result in a net gain or loss of genetic material, it is termed a balanced translocation and may not cause disease in carriers. However, it can lead to unbalanced gametes and cause disorders in offspring [10]. In a cancer context, a classic example is the formation of the BCR-ABL1 fusion gene, where the ABL1 proto-oncogene from chromosome 9 is juxtaposed with the BCR gene on chromosome 22, resulting in a constitutively active tyrosine kinase that drives leukemogenesis [8].
Table 1: Types of Chromosomal Translocations Leading to Gene Fusion
| Translocation Type | Molecular Description | Genomic Consequence | Example Fusion (Disease) |
|---|---|---|---|
| Reciprocal | Exchange of segments between two different chromosomes | Can be balanced or unbalanced; may form hybrid genes | BCR-ABL1 [8] (Chronic Myeloid Leukemia) |
| Robertsonian | Fusion of two acrocentric chromosomes at the centromeres | Loss of short arms; one large metacentric chromosome is formed | Associated with increased risk of translocation Down syndrome [10] |
| Nonreciprocal | One-way transfer of genetic material to another chromosome | Unbalanced; results in gain or loss of genetic material | Implicated in Emanuel Syndrome [10] |
Interstitial Deletions
Interstitial deletions involve the loss of a segment of DNA from within a chromosome, not from the telomere. If the deleted region is between two genes, the deletion can bring the promoter or regulatory sequences of one gene into close proximity with the coding region of another, effectively fusing them into a single transcriptional unit [8]. A key example is the PAX7-FOXO1 fusion gene in rhabdomyosarcoma, which arises from a deletion on chromosome 13 that bridges the two genes [8]. This fusion creates an oncogenic transcription factor that disrupts normal muscle cell development.
Chromosomal Inversions
Chromosomal inversions occur when a segment of a chromosome breaks, rotates 180 degrees, and reinserts back into the same location. When the breakpoints of this inversion lie within two different genes, it can fuse parts of these genes while keeping the overall chromosome structure relatively intact [8]. An inversion on chromosome 8, for instance, can lead to the FGFR1::PLAG1 fusion gene, which is responsible for certain pleomorphic adenomas and myoepithelial carcinomas [8]. This inversion places the fibroblast growth factor receptor 1 gene under the control of the PLAG1 promoter, leading to its aberrant expression.
The following diagram illustrates these three primary mechanisms at the chromosomal level.
Alternative RNA-Level Mechanisms
While DNA-level rearrangements are the most common cause, gene fusions can also form at the RNA level through trans-splicing, where two separate RNA transcripts from different genes are spliced together into a single chimeric mRNA [8]. An example is the JAZF1-JJAZ1 fusion, detected in endometrial stromal sarcomas [8]. Another mechanism is transcription-induced gene fusion, where read-through transcription of adjacent genes produces a single fusion transcript without an underlying genomic rearrangement [11] [9].
Quantitative Analysis of Gene Fusion Landscapes
Large-scale genomic studies have revealed that the frequency and recurrence of gene fusions vary significantly across cancer types. Hematologic malignancies and soft tissue sarcomas show the highest prevalence, with gene fusions driving over 50% of leukemias and one-third of soft tissue tumors [9]. In contrast, their prevalence in common epithelial cancers is generally lower but remains clinically significant.
Table 2: Gene Fusion Prevalence and Functional Impact Across Cancers
| Cancer Type | Prevalence of Pathogenic Fusions | Example Oncogenic Fusion(s) | Primary Functional Consequence |
|---|---|---|---|
| Prostate Cancer | ~50% (TMPRSS2-ERG fusion alone) | TMPRSS2-ERG [9] | Overexpression of ERG transcription factor |
| Leukemias & Lymphomas | >50% | BCR-ABL1, ETV6-RUNX1, MLL fusions [9] | Constitutive kinase activity or altered transcription |
| Soft Tissue Tumors | ~33% | EWSR1-FLI1 (Ewing Sarcoma) [12] | Chimeric transcription factor driving proliferation |
| Lung Adenocarcinoma | ~6% (EML4-ALK fusion) | EML4-ALK [9] | Constitutive ALK kinase activity |
| Pilocytic Astrocytoma | High | KIAA1549-BRAF [12] | Constitutive BRAF kinase activity driving MAPK pathway |
| Lipoblastoma | Recurrent | COL3A1-PLAG1 [12] | Promoter swapping leading to PLAG1 oncogene activation |
Bioinformatic analyses of gene fusion networks have uncovered key patterns. Most fusion genes partner with a single other gene, while a few, such as MLL (KMT2A), are highly promiscuous and can fuse with over 60 different partners [9]. Furthermore, gene fusion networks often exhibit cancer-type specificity; for instance, fusions in hematopoietic and mesenchymal cancers tend to cluster in distinct regions of the overall network [9].
Experimental Protocols for Fusion Gene Detection
The accurate detection of gene fusions is critical for cancer diagnosis, prognosis, and therapeutic targeting. The following protocols outline standard and next-generation methods.
Protocol: RNA Sequencing for Genome-Wide Fusion Detection
RNA sequencing (RNA-seq) is a powerful, untargeted method for discovering known and novel fusion transcripts across the entire transcriptome. A prospective study on pediatric cancers demonstrated that implementing RNA-seq increased the diagnostic yield of gene fusion detection by 38-39% compared to traditional diagnostic techniques alone [12].
Workflow Overview:
- Sample Preparation & RNA Extraction: Obtain fresh-frozen tissue or bone marrow. Isolate total RNA using a column-based or phenol-chloroform extraction method. Assess RNA integrity (RIN > 7.0 is recommended).
- Library Preparation: Deplete ribosomal RNA (ribo-depletion) to enrich for coding and non-ribosomal transcripts. Convert purified RNA into a sequencing library using a strand-specific kit (e.g., Illumina TruSeq Stranded Total RNA).
- High-Throughput Sequencing: Sequence the libraries on a platform such as Illumina NovaSeq 6000, aiming for a minimum of 80-100 million uniquely mapped reads per sample to ensure sensitivity for low-abundance fusions [12].
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to the reference genome using a splice-aware aligner (e.g., STAR).
- Fusion Calling: Process aligned reads with a dedicated fusion detection tool such as STAR-Fusion (version 1.6.0 or later) [12].
- Annotation & Filtering: Annotate candidate fusions with known databases and filter out common artifacts. Prioritize protein-protein coding fusions and those with supporting reads spanning the breakpoint.
- Validation: Confirm high-priority, novel fusions using an independent technique such as RT-PCR or FISH.
Protocol: Fluorescence In Situ Hybridization (FISH)
FISH is a targeted cytogenetic technique that uses fluorescently labeled DNA probes to visualize specific genetic regions on metaphase chromosomes or in interphase nuclei. It is a gold standard for validating fusion events detected by other methods.
Workflow Overview:
- Sample Preparation: Prepare metaphase chromosomes from dividing cells or use interphase nuclei from tissue sections (e.g., formalin-fixed, paraffin-embedded - FFPE).
- Probe Selection:
- Break-Apart Probes: Two probes flanking a common breakpoint region in a gene (e.g., EWSR1). In a normal cell, the signals are co-localized (yellow). A rearrangement separates the signals (red and green).
- Fusion Probes: Two probes labeled in different colors that bind to the two genes involved in a specific fusion (e.g., BCR and ABL1). A positive result is indicated by the juxtaposition (overlap) of the two signals.
- Hybridization: Denature the probe and sample DNA simultaneously. Incubate to allow the probe to hybridize to its complementary target sequence.
- Washing and Detection: Wash away unbound probe. If using indirect detection, apply fluorescently labeled antibodies. Counterstain with DAPI to visualize the nucleus.
- Microscopy and Analysis: Visualize signals using a fluorescence microscope. Score a sufficient number of cells (e.g., 200 nuclei) for the presence of split or fused signals to determine if the fusion is present.
Protocol: Electrochemical Biosensing for Fusion Gene Detection
Electrochemical (EC) biosensors are emerging as a rapid, cost-effective, and highly sensitive alternative for detecting specific fusion gene sequences, showing great promise for point-of-care diagnostics [13].
Workflow Overview:
- Biosensor Fabrication: Functionalize a gold or screen-printed carbon electrode surface with a capture probe. This is typically a single-stranded DNA (ssDNA) sequence complementary to a specific region of the target fusion gene RNA or DNA (e.g., the unique breakpoint sequence of BCR-ABL1). Use self-assembled monolayers (SAMs) like thiolated DNA to anchor the probe on gold electrodes.
- Sample Processing and Target Amplification: Extract RNA or DNA from patient blood or tissue. For high sensitivity, amplify the target sequence using RT-PCR or isothermal amplification (e.g., LAMP, RPA). Amplicons are often labeled with an electroactive tag (e.g., methylene blue) during amplification.
- Hybridization and Assay: Incubate the prepared sample with the functionalized electrode. The target fusion gene sequence will hybridize with the immobilized capture probe, bringing the electroactive tag close to the electrode surface.
- Electrochemical Signal Transduction: Perform an electrochemical measurement, such as differential pulse voltammetry (DPV) or electrochemical impedance spectroscopy (EIS). Hybridization events cause a measurable change in current (in DPV) or impedance (in EIS).
- Signal Quantification: The magnitude of the electrochemical signal (e.g., current peak in DPV) is proportional to the amount of captured target, allowing for quantification of the fusion transcript.
The following diagram illustrates a generalized workflow for fusion gene analysis, integrating both sequencing and biosensor approaches.
The Scientist's Toolkit: Research Reagent Solutions
Successful detection and analysis of gene fusions rely on a suite of specialized reagents and tools.
Table 3: Essential Reagents and Materials for Fusion Gene Research
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Ribo-Depletion Reagents | Removes abundant ribosomal RNA during library prep, enriching for mRNA and non-coding RNA for RNA-seq. | Essential for obtaining high-quality, comprehensive transcriptome data from total RNA extracts [12]. |
| Strand-Specific Library Prep Kits | Preserves the original strand orientation of RNA transcripts during cDNA synthesis and library construction. | Critical for accurately determining the architecture and correct partner orientation of fusion transcripts in RNA-seq [12]. |
| Break-Apart FISH Probes | Fluorescently labeled DNA probes designed to flank a known common breakpoint region in a gene of interest. | Detects rearrangements of promiscuous genes like EWSR1 or ALK without prior knowledge of the fusion partner [12]. |
| Fusion-Specific FISH Probes | Two differently colored probes designed to bind the two specific genes involved in a known fusion. | Confirms the presence of a specific fusion, such as BCR-ABL1, by visualizing signal co-localization [10]. |
| Thiolated DNA Capture Probes | Single-stranded DNA probes with a thiol group that forms a self-assembled monolayer (SAM) on gold electrode surfaces. | Serves as the recognition element in an electrochemical biosensor for a specific fusion gene target [13]. |
| Electroactive Labels (e.g., Methylene Blue) | Redox-active molecules that produce a measurable current change upon a reduction-oxidation reaction at the electrode. | Used to label target amplicons; a change in signal upon hybridization indicates detection of the fusion sequence [13] [14]. |
| PRL-3 inhibitor I | PRL-3 inhibitor I, CAS:893449-38-2, MF:C17H11Br2NO2S2, MW:485.2 g/mol | Chemical Reagent |
| BRD4 degrader AT1 | BRD4 degrader AT1, MF:C48H58ClN9O5S3, MW:972.7 g/mol | Chemical Reagent |
Implications for Electrochemical Biosensor Development
Understanding the precise mechanisms of gene fusion formation is paramount for designing effective electrochemical detection strategies. The knowledge that specific fusion breakpoints are consistent in certain cancers (e.g., the BCR-ABL1 breakpoint in CML) allows for the design of highly specific thiolated DNA capture probes that are complementary to these unique junctional sequences [13] [8]. This specificity is crucial for distinguishing the pathogenic fusion from wild-type transcripts in a patient sample.
Furthermore, the documented high prevalence of kinase fusions across diverse cancers (e.g., involving ALK, ROS1, RET, and NTRK) establishes a strong rationale for developing multiplexed electrochemical biosensors [9]. Such a device could simultaneously screen for multiple therapeutically relevant fusion targets from a single sample, aligning with the clinical need for comprehensive molecular profiling. The robust nature and potential for miniaturization of electrochemical platforms address key limitations of traditional methods, offering a path toward rapid, point-of-care fusion gene diagnostics that could greatly expand access to precision oncology [13] [14].
Electrochemical biosensing represents a revolutionary methodology that provides rapid, cost-effective, and highly sensitive detection of biological molecules. This technique measures electrical signals generated by chemical reactions at the interface of an electrode and a biological sample, where electron transfer provides quantitative information about specific biomarkers [14]. In the context of cancer diagnostics, particularly for fusion gene detection, electrochemical biosensors translate the specific recognition of nucleic acid sequences into an analytically readable electrical signal, enabling precise molecular analysis essential for precision oncology [15] [14].
The superior efficacy of electrochemical biosensors compared to conventional techniques lies in their ability to detect cancer biomarkers with enhanced specificity and sensitivity. These platforms are highly adaptable to miniaturization, allowing for the development of portable, point-of-care diagnostic devices that can bring cancer screening closer to patients. Furthermore, the integration of electrochemical systems with advanced technologies such as microfluidics and nanotechnology enhances their potential for rapid and precise detection of fusion genes, which are critical oncogenic drivers in many cancer types [14].
Fundamental Principles
Core Mechanism of Signal Transduction
The underlying principle of electrochemical detection involves monitoring electrical currents generated from redox reactions. When a chemical reaction involving electron transfer occurs, the resulting current provides quantitative information about the concentration of the target species [14]. In a typical electrochemical cell, an applied potential between working and reference electrodes drives redox reactions, with oxidation occurring at the anode (electron loss) and reduction at the cathode (electron gain).
For fusion gene detection, this principle is harnessed through biosensors functionalized with specific recognition elements (e.g., DNA probes) complementary to target fusion sequences. Hybridization events between probe and target DNA induce measurable changes in electrical properties, including current, potential, or impedance, effectively transducing molecular recognition into an analytical signal.
Key Electrochemical Techniques
Various electrochemical techniques are employed in biosensing applications, each with distinct advantages for specific detection scenarios:
Voltammetry: The applied potential to the working electrode is varied in a controlled manner while monitoring the resulting current. Different voltammetric methods provide specific benefits for biosensing applications [14].
Amperometry: Measures current at a fixed potential over time, proportional to analyte concentration.
Potentiometry: Monitors potential difference between electrodes under conditions of zero current.
Electrochemical Impedance Spectroscopy (EIS): Characterizes the impedance of the electrode-electrolyte interface, highly sensitive to surface binding events.
Application Notes: Fusion Gene Detection
Experimental Protocol: Electrochemical Detection of NTRK Gene Fusions
Principle: This protocol describes a sandwich hybridization assay for detecting NTRK gene fusions using screen-printed gold electrodes functionalized with specific capture and signal probes.
Materials:
- Screen-printed gold electrodes (SPGEs)
- Thiol-modified DNA capture probes complementary to NTRK fusion sequences
- RNA extracts from patient samples
- HRP-labeled signaling probes
- TMB substrate solution
- Phosphate buffer saline (PBS, 0.1 M, pH 7.4)
- Differential pulse voltammetry (DPV) instrument
Procedure:
Electrode Pretreatment:
- Clean SPGEs by cycling in 0.5 M Hâ‚‚SOâ‚„ from 0 to +1.5 V until stable voltammogram obtained
- Rinse thoroughly with deionized water and dry under nitrogen stream
Probe Immobilization:
- Incubate electrodes with 20 μL of 1 μM thiolated capture probe in PBS for 2 hours at 25°C
- Passivate with 1 mM MCH for 30 minutes to minimize non-specific adsorption
- Wash with PBS to remove unbound probes
Target Hybridization:
- Apply 25 μL of RNA sample (diluted in hybridization buffer) to functionalized electrode
- Incubate at 37°C for 60 minutes with 80% humidity
- Wash stringently with PBS-Tween (0.05%) to remove non-specifically bound RNA
Signal Amplification:
- Incubate with HRP-conjugated detection probe (0.5 μM) for 45 minutes at 37°C
- Wash to remove unbound detection probe
- Add TMB substrate solution and incubate for 10 minutes
Electrochemical Measurement:
- Apply differential pulse voltammetry parameters:
- Potential range: -0.2 to +0.6 V
- Pulse amplitude: 50 mV
- Pulse width: 50 ms
- Scan rate: 20 mV/s
- Measure reduction current of TMB product at +0.2 V
- Compare against calibration curve for quantification
- Apply differential pulse voltammetry parameters:
Performance Data for Fusion Gene Detection
Table 1: Analytical Performance of Electrochemical Biosensors for Fusion Gene Detection
| Fusion Gene | Detection Technique | Linear Range (M) | LOD (pM) | Assay Time (min) | Clinical Sample Type |
|---|---|---|---|---|---|
| EML4-ALK | DPV with AuNPs | 10â»Â¹âµ - 10â»â¹ | 0.1 | 90 | Plasma-derived RNA |
| TMPRSS2-ERG | EIS with graphene | 10â»Â¹â´ - 10â»â¸ | 1.0 | 120 | Cell lines |
| BCR-ABL1 | Amperometry with CNTs | 10â»Â¹Â³ - 10â»â· | 0.5 | 75 | Serum RNA |
| NTRK1 | Voltammetry with MB | 10â»Â¹â¶ - 10â»Â¹â° | 0.01 | 60 | Tissue biopsy |
Comparison with Conventional Methods
Table 2: Method Comparison for Fusion Gene Detection in Cancer Diagnostics
| Parameter | Electrochemical Biosensor | RNA-Seq with Arriba | RT-PCR | FISH |
|---|---|---|---|---|
| Sensitivity | 0.01-1 pM | 88/150 fusions | 1-10 pM | Moderate |
| Specificity | >95% | High | High | High |
| Turnaround Time | 60-120 min | >24 hours | 3-4 hours | 2-3 days |
| Cost per Sample | $10-20 | $500-1000 | $50-100 | $150-200 |
| RNA Input | 1-10 ng | 100-1000 ng | 10-100 ng | N/A |
| Equipment Needs | Portable potentiostat | High-performance computing | Thermal cycler | Fluorescence microscope |
| Multiplexing Capability | High | Very High | Moderate | Low |
Research Reagent Solutions
Table 3: Essential Research Reagents for Electrochemical Fusion Gene Detection
| Reagent/Material | Function | Example Specifications |
|---|---|---|
| Screen-printed electrodes | Signal transduction platform | Gold, carbon, or graphene working electrode; integrated reference/counter electrodes |
| Thiol-modified DNA probes | Capture fusion gene sequences | 25-30 nt, complementary to fusion breakpoints, 5'-thiol modification, HPLC purified |
| Redox mediators | Generate electrochemical signal | Methylene blue, ferricyanide, TMB-HRP system |
| Nanomaterial enhancers | Signal amplification | 20-40 nm gold nanoparticles, graphene oxide, carbon nanotubes |
| Blocking agents | Reduce non-specific binding | MCH, BSA, salmon sperm DNA, Tween-20 |
| Hybridization buffers | Optimize target-probe binding | SSC buffer with formamide, dextran sulfate, Denhardt's solution |
Experimental Workflow Visualization
Electrochemical Fusion Gene Detection Workflow
Biosensing Principle and Interference Factors
Electrochemical biosensors represent a transformative approach in oncology, offering a powerful alternative to conventional diagnostic methods for the detection of cancer biomarkers, including fusion genes. These devices integrate a biological recognition element (such as a nucleic acid probe for a specific fusion gene) with an electrochemical transducer that converts a biological binding event into a quantifiable electrical signal [14] [16]. The global burden of cancer, with millions of new cases and deaths annually, underscores the urgent need for diagnostic tools that enable earlier detection and intervention, which significantly improves patient survival rates [17] [7]. Traditional diagnostic techniques, including tissue biopsy, computed tomography (CT), and MRI,, despite their clinical utility, often face limitations such as high cost, invasiveness, time-intensive procedures, and limited sensitivity for early-stage detection [14] [18] [19]. In contrast, electrochemical biosensors are emerging as a cornerstone of point-of-care (PoC) diagnostics, providing rapid, cost-effective, and highly sensitive detection of specific cancer biomarkers with potential for decentralized testing [14] [6] [20].
Comparative Advantage Analysis
The transition from traditional diagnostic methodologies to advanced electrochemical biosensors is driven by significant improvements in key performance parameters. The following table summarizes the comparative advantages of electrochemical biosensors across critical diagnostic criteria.
Table 1: Comparative Analysis of Cancer Diagnostic Methods
| Diagnostic Method | Sensitivity | Analysis Speed | Cost | Potential for Miniaturization |
|---|---|---|---|---|
| Tissue Biopsy | High (but invasive) | Slow (days for results) | High | Low [18] |
| Mammography/CT/MRI | Moderate (limited for early stages) | Moderate to Fast | High | Low [19] |
| ELISA | Moderate (detection limit ~10â·/μL for exosomes) | Moderate (several hours) | Moderate | Moderate [16] |
| PCR/qRT-PCR | High | Slow (hours, requires thermal cycling) | High | Low to Moderate [21] |
| Electrochemical Biosensors | Very High (detects attomolar-femtomolar concentrations) [22] | Very Fast (minutes to seconds) [14] | Low [14] [7] | High (Lab-on-a-Chip platforms) [6] [21] |
Beyond the general advantages, the quantitative performance of electrochemical biosensors is exemplified in specific research applications, particularly for detecting low-abundance biomarkers like fusion gene components or exosomal cargo.
Table 2: Performance Metrics of Selected Electrochemical Biosensors in Cancer Detection
| Target Biomarker | Sensor Type/Technique | Reported Sensitivity (Limit of Detection) | Linear Detection Range | Reference |
|---|---|---|---|---|
| MicroRNA (miR-21) | Homogeneous, label-free with G-triplex/MB | [22] | ||
| Tumor-Derived Exosomes | Various electrochemical (voltammetric, impedimetric) | [16] | ||
| HER2 Protein | Nanomaterial-based immunosensor | [19] | ||
| Nucleic Acids (General) | Lab-on-a-Chip with electrochemical detection | Down to a single copy for mRNA markers [18] | [18] |
Experimental Protocols for Fusion Gene Detection
The following protocols provide a framework for developing electrochemical biosensors tailored for the detection of fusion genes, which are critical biomarkers in several cancer types.
Protocol 1: Fabrication of a Miniaturized Electrode Biochip
This protocol details the creation of a miniaturized, multi-electrode biochip suitable for genetic sensing applications [21].
I. Materials
- Substrate: Double-sided polished borosilicate glass wafer (150 mm diameter, 600 μm thickness).
- Metallic Layers: Chromium (Cr, 5 nm for adhesion), Gold (Au, 200 nm), Platinum (Pt, 200 nm).
- Photolithography: Positive-tone photoresist, HMDS primer, and corresponding developers/etchants.
- Passivation: Silicon Dioxide (SiOâ‚‚).
- Equipment: UV mask aligner, thermal evaporator, wet chemical etching bench.
II. Procedure
- Wafer Cleaning: Clean the glass wafer in a buffered hydrofluoric acid (HF) bath for 20 seconds, followed by rinsing with deionized water and drying.
- Deposition of Adhesion and Metal Layers:
- Use a thermal evaporator to deposit a 5 nm Cr layer followed by a 200 nm Au layer onto the clean wafer.
- Photolithography Patterning (First Mask - M1):
- Prime the wafer with HMDS at 150°C.
- Spin-coat a ~2 μm layer of positive-tone photoresist.
- Soft-bake at 100°C for 1 minute.
- Align and expose the wafer to UV light through mask M1 (defines reference and counter electrodes).
- Develop the photoresist to remove exposed areas.
- Perform wet chemical etching to transfer the pattern first to the Au and then to the Cr layers.
- Strip the remaining photoresist with acetone.
- Patterning of the Working Electrode (Second Mask - M2):
- Coat the wafer again with photoresist.
- Align and expose the wafer to UV light through dark-field mask M2 (defines the working electrode area).
- Develop the photoresist.
- Deposit a 5 nm Cr layer followed by a 200 nm Pt layer via thermal evaporation.
- Perform a lift-off process in acetone, leaving the Pt working electrode feature.
- Passivation Layer Deposition and Patterning (Third Mask - M3):
- Deposit a SiOâ‚‚ layer over the entire wafer.
- Coat with photoresist and expose through mask M3 to define the active electrode areas.
- Etch the SiOâ‚‚ to open contact windows.
- Dicing and Packaging: Dice the wafer into individual chips and package for electrical connection and fluidic interfacing.
III. Diagram: Biochip Fabrication Workflow
Protocol 2: Functional Nucleic Acid-Based Homogeneous miRNA Detection
This protocol describes a label-free, homogeneous method for detecting microRNA (e.g., a fusion gene transcript) using a functional nucleic acid probe and an integrated microelectrode (IME) [22].
I. Materials
- Integrated Microelectrode (IME): Comprising a 15 μm gold wire working electrode, carbon rod counter electrode, and homemade Ag/AgCl reference electrode assembled in a three-channel glass microtube.
- Probe: Functional nucleic acid probe (e.g., G-triplex DNA with a caged complementary sequence for the target miRNA).
- Signal Molecule: Methylene blue (MB).
- Buffer: 10 mM phosphate buffer (pH 7.2) with 100 mM KCl.
- Target: Synthetic target miRNA (e.g., miR-21) or extracted RNA sample.
II. Procedure
- IME Preparation and Characterization:
- Fabricate the IME as described in the referenced literature [22].
- Characterize the IME performance using square-wave voltammetry (SWV) in a 100 μM MB solution to confirm a clear oxidation peak.
- Assay Execution:
- In a microcentrifuge tube, mix the functional nucleic acid probe with the target miRNA in phosphate buffer.
- Incubate the mixture at room temperature for a predetermined time (e.g., 30-60 minutes) to allow for hybridization and probe conformation change.
- Add MB to the mixture to a final concentration of 100 μM.
- Transfer a microliter-scale volume (e.g., 2-5 μL) of the final mixture to the IME for measurement.
- Signal Measurement:
- Perform SWV measurement using the IME.
- Record the reduction in the peak current of free MB compared to a blank (no target) control.
- Data Analysis:
- Quantify the target concentration based on the relative decrease in peak current, using a calibration curve established with known concentrations of the target miRNA.
III. Diagram: Homogeneous miRNA Detection Mechanism
The Scientist's Toolkit: Essential Research Reagent Solutions
The performance of electrochemical biosensors is critically dependent on the careful selection of materials and reagents. The following table outlines key components and their functions in sensor development.
Table 3: Essential Research Reagents and Materials for Electrochemical Biosensor Development
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| MXene (e.g., Ti₃C₂Tₓ) [17] | Sensor interface/electrode modifier | High electrical conductivity, chemical stability, functional versatility for enhanced signal transduction. |
| Thiol-modified Oligonucleotides [21] | Probe immobilization | Forms self-assembled monolayers (SAMs) on gold or platinum electrodes, enabling stable surface functionalization. |
| G-triplex (G3) DNA [22] | Signal transduction probe | Forms a stable complex with methylene blue (MB) in solution, leading to a measurable change in diffusion current. |
| Methylene Blue (MB) [22] | Electroactive label | Redox indicator whose diffusion coefficient and current signal change upon binding to released G3 DNA. |
| Platinum (Pt) & Gold (Au) Electrodes [21] | Working electrode substrate | Excellent conductivity, chemical stability, and high affinity for thiol-modified biomolecules for robust sensor fabrication. |
| Phosphate Buffered Saline (PBS) [21] | Electrolyte/Buffer | Provides a stable ionic strength and pH environment for electrochemical measurements and biochemical reactions. |
| BRD6688 | BRD6688, MF:C16H18N4O, MW:282.34 g/mol | Chemical Reagent |
| Candicidin D | Candicidin D, CAS:39372-30-0, MF:C59H84N2O18, MW:1109.3 g/mol | Chemical Reagent |
Electrochemical biosensors, with their superior sensitivity, rapid analysis, cost-effectiveness, and capacity for miniaturization, represent a paradigm shift in cancer diagnostics. The detailed protocols and material insights provided herein offer a practical roadmap for researchers aiming to develop next-generation detection platforms for fusion genes and other critical cancer biomarkers. The ongoing integration of advanced nanomaterials, innovative probe designs, and Lab-on-a-Chip technologies will further solidify the role of these sensors in enabling early cancer detection and personalized medicine.
Designing and Engineering Electrochemical Genosensors for Fusion Gene Detection
The reliable detection of fusion genes is a critical component of modern precision oncology, as these hybrid genes, formed through chromosomal rearrangements such as translocations, deletions, or inversions, act as potent drivers of malignant transformation in various cancers [23] [24]. The identification of targetable fusions in genes like ALK, ROS1, RET, and NTRK directly influences therapeutic decision-making, enabling treatment with specific tyrosine kinase inhibitors [23] [15]. However, the clinical utility of these biomarkers hinges on the accuracy of the detection methods, which is profoundly influenced by the initial probe immobilization strategies used to capture fusion gene transcripts and amplicons.
Probe immobilization forms the foundational step in numerous molecular assays, including microarrays, next-generation sequencing (NGS) library preparation, and biosensor development. The method of immobilization dictates the probe's surface density, orientation, and accessibility, thereby directly impacting the efficiency and specificity of target capture [25]. In the context of fusion gene detection, where sequence homology can be complex and expression levels variable, optimized immobilization strategies are paramount for achieving high sensitivity and minimizing false positives and negatives. This document details advanced protocols and application notes for immobilizing probes designed to capture fusion gene targets, with a specific focus on applications within electrochemical detection platforms for cancer diagnosis research.
Fusion Gene Detection Methodologies
The choice between different broad methodologies dictates the optimal probe design and immobilization strategy. The two primary approaches for targeted sequencing are hybridization capture and amplicon sequencing, each with distinct advantages [26].
Table 1: Comparison of Hybridization Capture and Amplicon Sequencing for Fusion Gene Detection
| Feature | Hybridization Capture | Amplicon Sequencing |
|---|---|---|
| Principle | Solution-based hybridization of biotinylated DNA/RNA probes to target, followed by immobilization on streptavidin beads | PCR amplification using target-specific primers |
| Number of Targets | Virtually unlimited by panel size | Flexible, but usually fewer than 10,000 amplicons |
| Workflow | More steps and time | Fewer steps and less time |
| Cost per Sample | Varies | Generally lower |
| On-target Rate | High uniformity across targets | Naturally high, but uniformity can vary |
| Best For | Large target regions, exome sequencing, rare variant identification | Smaller target panels, germline SNPs/indels, known fusion verification |
For electrochemical biosensors, the detection principle revolves around the translation of a specific biorecognition event (e.g., DNA hybridization) into a measurable electrical signal [27] [14] [28]. These platforms often employ a three-electrode system where the working electrode is functionalized with a capture probe. Upon hybridization with the target fusion gene sequence, a change in electrochemical properties—such as current, potential, or impedance—is measured. The immobilization of the DNA capture probe onto the electrode surface is a critical determinant of the sensor's performance, affecting its sensitivity, specificity, and reproducibility [28].
Experimental Protocols
Protocol 1: Immobilization of Single-Stranded DNA (ssDNA) Probes on Gold Electrodes for Electrochemical Detection
This protocol describes a robust method for covalently immobilizing thiol-modified ssDNA capture probes onto gold electrodes, a common setup in electrochemical genosensors for detecting fusion transcripts like PML/RARα or BCR/ABL [28].
Materials:
- Working Electrode: Gold disk electrode (e.g., 2 mm diameter).
- Capture Probe: Thiol-modified ssDNA probe (e.g., 5'-HS-(CH₂)₆-[Gene-Specific Sequence]-3').
- Chemicals: 6-Mercapto-1-hexanol (MCH), Tris(2-carboxyethyl)phosphine hydrochloride (TCEP), Potassium ferricyanide (K₃[Fe(CN)₆]), Potassium ferrocyanide (K₄[Fe(CN)₆]), Phosphate Buffered Saline (PBS, pH 7.4).
- Equipment: Potentiostat, electrochemical cell.
Procedure:
- Electrode Pretreatment: Clean the gold electrode by polishing with 0.05 µm alumina slurry, followed by sequential sonication in ethanol and deionized water for 5 minutes each. Electrochemically clean by performing cyclic voltammetry (CV) in 0.5 M H₂SO₄ from -0.2 V to +1.5 V until a stable voltammogram is obtained.
- Probe Reduction: Reduce the thiolated ssDNA probe (100 µM) in 10 mM TCEP for 1 hour at room temperature to cleave any disulfide bonds.
- Probe Immobilization: Deposit 10 µL of the reduced probe solution (1 µM in PBS) onto the cleaned gold surface and incubate in a humidified chamber for 16 hours at 4°C.
- Backfilling: Rinse the electrode gently with PBS to remove unbound probes. Incubate with 1 mM MCH in PBS for 1 hour to passivate the remaining gold surface, which minimizes non-specific adsorption and improves probe orientation.
- Hybridization Assay: Incubate the functionalized electrode with the target DNA or RNA sample (e.g., amplified fusion gene transcripts) in a suitable hybridization buffer (e.g., 5x SSC + 0.1% Tween-20) for 30-60 minutes at a defined temperature.
- Electrochemical Measurement: Perform electrochemical measurements, such as Differential Pulse Voltammetry (DPV) or Electrochemical Impedance Spectroscopy (EIS), in a solution containing a redox couple like 5 mM [Fe(CN)₆]³â»/â´â». The hybridization event will cause a measurable change in the current or impedance.
Protocol 2: Functionalization of Magnetic Beads with Recombinant Fusion Proteins for Antibody-Free Capture
This innovative protocol leverages genetic engineering to create a self-immobilizing capture system, avoiding the need for complex surface chemistry [25]. It involves expressing a fusion protein between a hydrophobin (a powerful self-assembling fungal protein) and a single-chain variable fragment (ScFv) of an antibody or a specific DNA-binding domain.
Materials:
- Vmh2-ScFv Fusion Protein: Recombinantly expressed in E. coli and purified from inclusion bodies [25].
- Magnetic Beads: Plain polystyrene or carboxyl-modified magnetic beads (MBs).
- Buffers: Refolding buffer (e.g., 100 mM Tris-HCl, 0.5 M L-Arginine, 2 mM GSH/GSSG, pH 8.0), PBS.
Procedure:
- Protein Refolding: Solubilize the inclusion bodies containing the Vmh2-ScFv fusion protein in a denaturing buffer (e.g., 8 M urea). Refold the protein by rapid dilution into a refolding buffer and incubate for 24-48 hours at 4°C.
- Beads Functionalization: Incubate the refolded Vmh2-ScFv protein (e.g., 50 µg/mL) with the magnetic beads in PBS for 2 hours at room temperature with gentle agitation. The hydrophobin (Vmh2) moiety will spontaneously and irreversibly adsorb to the hydrophobic surface of the beads.
- Washing: Wash the beads three times with PBS to remove any unbound protein.
- Target Capture: The ScFv moiety is now displayed on the bead surface. Incubate the functionalized beads with the sample containing the target antigen (e.g., a fusion protein) or with amplicons that have been tagged with the corresponding epitope for 1 hour.
- Detection: After magnetic separation and washing, the captured target can be detected. In an electrochemical setup, this can be achieved by using an enzyme-conjugated secondary antibody (e.g., HRP-STX) and an appropriate substrate (e.g., TMB or Hâ‚‚Oâ‚‚/ABTS), which generates an electroactive product [25].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Probe Immobilization and Fusion Gene Capture
| Research Reagent | Function & Application |
|---|---|
| Thiol-modified ssDNA | Allows for covalent attachment to gold surfaces via Au-S bonds; foundational for electrochemical DNA biosensors [28]. |
| Biotinylated DNA/RNA Probes | Used in hybridization capture; the biotin-streptavidin interaction enables immobilization on streptavidin-coated beads or surfaces for NGS [26]. |
| Hydrophobin-ScFv Fusion Protein | A self-assembling chimeric protein for direct, oriented, and antibody-free immobilization of recognition elements on various surfaces [25]. |
| 6-Mercapto-1-hexanol (MCH) | A passivating alkanethiol used to create a well-ordered self-assembled monolayer on gold, reducing non-specific binding and improving probe accessibility [28]. |
| Streptavidin-coated Magnetic Beads | Solid support for capturing biotinylated probes or targets, enabling easy concentration and washing steps in library prep or sample preparation [26]. |
| Nano-porous Gold (NPG) Electrode | A transducer with high surface area-to-volume ratio, enhancing the immobilization capacity and the sensitivity of electrochemical biosensors [28]. |
| Cathepsin inhibitor 1 | Cathepsin inhibitor 1, MF:C20H24ClN5O2, MW:401.9 g/mol |
| Caylin-1 | Caylin-1, MF:C30H28Cl4N4O4, MW:650.4 g/mol |
Workflow and Data Analysis
The following diagram illustrates the core decision-making workflow and experimental process for selecting and implementing a probe immobilization strategy for fusion gene detection.
The successful execution of these protocols yields quantitative data critical for assay validation. Key performance metrics to analyze include:
- Limit of Detection (LOD): The lowest concentration of target that can be reliably distinguished. For example, a biosensor using hydrophobin-ScFv immobilization achieved an LOD of 1.7 pg/mL for saxitoxin, demonstrating high sensitivity [25].
- Signal-to-Noise Ratio: The ratio of the specific signal from a positive hybridization to the background signal from a negative control.
- Reproducibility: The coefficient of variation of the signal across multiple replicates of the same sample.
Table 3: Example Electrochemical Performance Metrics for Different Immobilization Strategies
| Immobilization Strategy | Target Fusion/Optimization | Reported LOD | Key Advantage |
|---|---|---|---|
| Thiolated DNA on Au | PML/RARα [28] | Sub-nanomolar range | Well-established, direct covalent linkage |
| Vmh2-ScFv on MBs | Marine toxins (Model System) [25] | 1.7 pg/mL | No surface derivatization, oriented immobilization |
| Biotin-Streptavidin | NGS panels (e.g., ALK, ROS1) [26] [29] | High on-target reads | Extreme binding affinity, versatile |
The strategic selection and optimization of probe immobilization are fundamental to the success of fusion gene detection in both biosensing and sequencing applications. As detailed in these protocols, methods range from traditional chemical conjugation (thiol-gold, biotin-streptavidin) to innovative biological approaches (hydrophobin fusions), each offering distinct advantages in terms of simplicity, orientation, and specificity. For researchers in cancer diagnostics, mastering these immobilization techniques is crucial for developing robust, sensitive, and reliable assays. The future of this field lies in the continued refinement of these strategies, particularly through the integration of novel nanomaterials and engineered proteins, to further enhance the capture efficiency and analytical performance required for the electrochemical detection of low-abundance fusion genes in complex clinical samples.
The electrochemical detection of fusion genes represents a critical frontier in the molecular diagnosis of cancer. Technologies enabling the rapid, sensitive, and specific identification of these genetic markers are essential for early diagnosis, prognostic stratification, and treatment monitoring. Conventional detection methods, including quantitative reverse transcription-polymerase chain reaction (qRT-PCR) and fluorescence in situ hybridization (FISH), face limitations such as time-consuming protocols, requirement for sophisticated instrumentation, and high costs, restricting their utility in point-of-care settings [30] [31]. Electrochemical biosensors have emerged as a powerful alternative, offering the potential for rapid, low-cost, and highly sensitive detection. The integration of nanomaterials such as graphene, carbon nanotubes (CNTs), and metal nanoparticles into these sensing platforms has been transformative. These materials confer significant signal amplification by enhancing electrical conductivity, increasing the electroactive surface area for probe immobilization, and improving catalytic activity, thereby pushing the limits of detection for low-abundance fusion genes relevant to cancer diagnostics [32] [33] [34].
Performance of Nanomaterial-Enhanced Platforms
The table below summarizes the performance characteristics of various nanomaterial-enhanced electrochemical biosensors developed for the detection of cancer-related biomarkers, including fusion genes.
Table 1: Performance Summary of Selected Nanomaterial-Enhanced Electrochemical Biosensors
| Target Analyte | Nanomaterial Platform | Detection Technique | Linear Range | Limit of Detection (LOD) | Reference |
|---|---|---|---|---|---|
| PML/RARα Fusion Gene (APL) | Carbon Dots/Graphene Oxide (CDs/GO) | Differential Pulse Voltammetry (DPV) | Not Specified | 83 pM | [30] |
| BCR/ABL Fusion Gene (CML) | Chitosan-Graphene/Polyaniline/AuNPs | Amperometry | 10 – 1000 pM | 2.11 pM | [34] |
| p16INK4a Gene | Polypyrrole-Graphene Nanofiber | Electrochemiluminescence (ECL) | 0.1 pM – 1 nM | 0.05 pM | [34] |
| miRNA-21 | AuNPs-Graphene / Cd²âº-TiPhosphate NPs | Differential Pulse Voltammetry (DPV) | 10â»Â¹â¸ – 10â»Â¹Â¹ M | 0.76 aM | [34] |
| Prostate-Specific Antigen (PSA) | SWNT Forest with CNT-Abâ‚‚-HRP Bioconjugates | Amperometry | Not Specified | 4 pg mLâ»Â¹ (100 amol mLâ»Â¹) | [35] |
| α-Fetoprotein (AFP) | MWCNT-HRP Multilayers | Chemiluminescence | Not Specified | 8.0 pg mLâ»Â¹ | [36] |
| Staphylococcus Aureus (Model Pathogen) | CNFs/AuNPs/Cys/MWCNT | Differential Pulse Voltammetry (DPV) | 10 – 10â· CFU mLâ»Â¹ | 2.8 CFU mLâ»Â¹ | [37] |
Experimental Protocol: Detection of PML/RARα Fusion Gene using a CDs/GO Nanocomposite Biosensor
This protocol details the fabrication and operation of an electrochemical DNA biosensor for the detection of the acute promyelocytic leukemia (APL)-associated PML/RARα fusion gene, based on a carbon dots/graphene oxide (CDs/GO) nanocomposite platform [30].
Principle
The biosensor operates on a "signal-off" mechanism. A single-stranded DNA (ssDNA) capture probe, complementary to the target PML/RARα gene sequence, is immobilized on the CDs/GO-modified electrode. Upon hybridization with the target DNA to form double-stranded DNA (dsDNA), the electrochemical indicator methylene blue (MB) exhibits reduced affinity for the dsDNA compared to the ssDNA capture probe. This hybridization event leads to a decrease in the MB Faradaic current, which is quantitatively measured using differential pulse voltammetry (DPV) [30].
Materials and Reagents
Table 2: Key Research Reagent Solutions
| Reagent/Material | Function/Description | Source/Example |
|---|---|---|
| Graphene Oxide (GO) | Platform for probe immobilization; provides large surface area and oxygen functional groups for binding. | Nanjing XFNANO Technology Co., Ltd. |
| Carbon Dots (CDs) | Enhance electron transfer and conductivity of the nanocomposite; provide carboxyl groups for biomolecule attachment. | Synthesized from carbon fibers. |
| Capture Probe DNA | 22-base sequence (5'-NH₂-GGTCTCAATGGCTGCCTCCCCG-3') for specific recognition of the PML/RARα fusion gene. | Custom synthesis from Takara. |
| Methylene Blue (MB) | Electrochemical indicator that differentially intercalates with ssDNA vs. dsDNA. | Sigma-Aldrich. |
| EDC & NHS | Cross-linking agents for covalent immobilization of amine-terminated DNA capture probes. | Sigma-Aldrich. |
| Phosphate Buffered Saline (PBS) | Electrolyte and washing buffer (0.1 M, pH 7.4). | Prepared from Naâ‚‚HPOâ‚„ and NaHâ‚‚POâ‚„. |
| Tris-EDTA (TE) Buffer | For preparation and storage of DNA stock solutions. | Prepared from Tris-HCl and EDTA. |
Step-by-Step Procedure
Step 1: Synthesis of CDs/GO Nanocomposite
- Prepare CDs from carbon fibers via acid oxidation and pyrolysis.
- Mix the prepared CDs with an aqueous dispersion of GO under vigorous stirring.
- The CDs attach to the GO sheets via π-π stacking interactions to form the CDs/GO nanocomposite, which can be produced in large quantities via this ex-situ method.
Step 2: Electrode Modification
- Polish a glassy carbon electrode (GCE) sequentially with 0.3 and 0.05 μm alumina slurry, followed by rinsing with deionized water and ethanol.
- Deposit a specific volume (e.g., 5-10 μL) of the homogeneous CDs/GO nanocomposite dispersion onto the clean GCE surface.
- Allow the electrode to dry at room temperature to form the CDs/GO/GCE, which serves as the enhanced sensing platform.
Step 3: Immobilization of Capture Probe
- Activate the carboxyl groups on the CDs/GO/GCE surface by incubating with a fresh mixture of 400 mM EDC and 100 mM NHS for 10 minutes.
- Rinse the electrode gently with PBS to remove excess EDC/NHS.
- Apply a solution of the amine-terminated capture probe DNA (e.g., 20 μL of 1 μM solution in PBS) onto the activated electrode surface.
- Incubate for 3 hours at 37°C to allow covalent amide bond formation, immobilizing the probe.
- Wash the electrode with 0.05% Tween-20 in PBS and pure PBS to remove physically adsorbed DNA strands.
Step 4: Target Hybridization and Detection
- Incubate the DNA probe-modified electrode with a solution containing the target DNA sequence (complementary, single-base mismatch, or non-complementary) for a defined period (e.g., 1 hour) at a controlled temperature to facilitate hybridization.
- Rinse the electrode thoroughly with PBS to remove unhybridized DNA.
- Immerse the electrode in an electrochemical cell containing PBS and a defined concentration of MB.
- Record DPV signals in the potential window from -0.2 to -0.5 V (vs. Ag/AgCl). The peak current of MB reduction is measured.
- The change in current signal before and after hybridization, or between complementary and mismatched targets, is used for quantitative and specific analysis.
Data Analysis
- Plot the DPV peak current against the concentration of the complementary target DNA to establish a calibration curve.
- The limit of detection (LOD) can be calculated using the formula LOD = 3σ/S, where σ is the standard deviation of the blank signal and S is the slope of the calibration curve.
- The biosensor's specificity is validated by comparing the signal from the fully complementary target to signals from single-base mismatch and non-complementary DNA sequences.
Signaling Pathway and Experimental Workflow
The following diagram illustrates the signaling pathway and experimental workflow for the nanomaterial-enhanced electrochemical detection of fusion genes.
Diagram 1: Workflow and Amplification Mechanism. This diagram outlines the key steps in fabricating and operating a nanomaterial-enhanced electrochemical biosensor, highlighting the core mechanisms of signal amplification provided by the nanomaterials.
Troubleshooting and Optimization Notes
- Non-specific Binding: If high background signals are observed, optimize the concentration of Tween-20 in washing buffers and ensure adequate blocking steps with agents like BSA are included [35].
- Reproducibility: To ensure consistent sensor-to-sensor performance, standardize the concentration and volume of the nanomaterial dispersion used for electrode modification, as well as the drying conditions [30] [37].
- Probe Density and Orientation: The sensitivity of the biosensor is highly dependent on the surface density and orientation of the capture probes. Systematic optimization of EDC/NHS concentration and probe immobilization time is recommended [31].
- Stability: The CDs/GO and similar nanomaterial-modified electrodes should be stored in a dry state at 4°C when not in use. The long-term stability can be monitored by periodically checking the DPV response of a standard MB solution.
Electrochemical biosensors represent a paradigm shift in the detection of cancer biomarkers, offering a powerful alternative to conventional methods like polymerase chain reaction (PCR) and enzyme-linked immunosorbent assay (ELISA) that often require expensive equipment, lengthy analysis times, and specialized laboratory facilities [7] [18]. These sensors transduce biological recognition events into quantifiable electrical signals through various techniques, with voltammetry, amperometry, and impedimetry being the most prominent. The integration of these detection methods with novel materials and fabrication technologies has positioned electrochemical biosensors as next-generation tools for cancer diagnosis, particularly for detecting fusion genes—hybrid genes formed by the joining of two previously separate genes, which serve as critical diagnostic and prognostic indicators in various cancers [13] [38]. This article provides application-focused notes and detailed protocols for implementing these electrochemical transduction techniques within the specific context of fusion gene detection for cancer diagnostics.
Electrochemical Techniques: Core Principles and Comparative Analysis
Fundamental Principles
Voltammetry measures current as a function of the applied potential, providing quantitative information about the analyte based on the potential at which redox reactions occur and the magnitude of the resulting current. Common modalities include Cyclic Voltammetry (CV) and Square Wave Voltammetry (SWV). CV is particularly useful for characterizing the electrochemical behavior of a system, while SWV offers superior sensitivity for quantitative analysis due to its effective background current suppression [7] [39]. Amperometry involves measuring the current at a constant applied potential over time, with the current being directly proportional to the concentration of the electroactive species. This technique is known for its high sensitivity and simplicity. Impedimetry, specifically Electrochemical Impedance Spectroscopy (EIS), measures the impedance (resistance to current flow) of an electrochemical system across a range of frequencies. It is exceptionally suited for label-free detection of binding events, such as DNA hybridization, as these events alter the interfacial properties of the electrode [7] [16].
Performance Comparison of Techniques
The table below summarizes the key characteristics, advantages, and limitations of these three primary electrochemical techniques in the context of biosensing.
Table 1: Comparative Analysis of Voltammetry, Amperometry, and Impedimetry
| Technique | Measured Quantity | Key Advantages | Key Limitations | Typical LOD in Fusion Gene Detection |
|---|---|---|---|---|
| Voltammetry | Current vs. Applied Potential | - High sensitivity (esp. SWV)- Can study redox mechanisms- Multi-analyte detection potential | - Can be affected by non-Faradaic processes- May require redox mediators | ~8-12 copies/mL for viral genes [40] |
| Amperometry | Current vs. Time at Constant Potential | - Very high sensitivity- Simple instrumentation and operation- Real-time monitoring capability | - Requires application of optimal potential- Primarily for electroactive analytes | Sub-micromolar range for small molecules; LOD depends heavily on signal amplification [7] |
| Impedimetry | Impedance vs. Frequency | - Label-free detection- Minimal sample preparation- Sensitive to surface modifications | - Can be influenced by non-specific binding- Data interpretation can be complex | Highly sensitive for exosome and protein detection [16] |
Application Notes: Electrochemical Detection of Fusion Genes
Fusion genes, such as BCR-ABL1 in chronic myeloid leukemia and EML4-ALK in non-small cell lung cancer, are well-established cancer drivers and therapeutic targets [13] [38]. Electrochemical biosensors offer a promising route for their detection, providing a versatile, rapid, and cost-effective platform that does not compromise on specificity or sensitivity [13]. A critical application is the discrimination between viral genome states, as demonstrated for HPV-16 in cervical cancer. The ratio of the E2 gene (often disrupted upon integration into the host genome) to the E6 gene (which is retained) serves as a surrogate marker for malignant transformation. Electrochemical duplex sensors can simultaneously quantify both genes, calculating the E2/E6 ratio to distinguish between episomal (cut-off >0.77) and integrated forms with 100% sensitivity and specificity [40].
A significant challenge in multiplexed electrochemical detection is resolving signals from multiple analytes with similar redox potentials. Artificial Intelligence (AI) and Machine Learning (ML) are emerging as powerful tools to address this. AI algorithms can process complex voltammetric data to deconvolute overlapping signals, significantly improving qualitative identification and quantitative analysis in mixtures that are otherwise indistinguishable using conventional methods [39].
Detailed Experimental Protocols
Protocol 1: Duplex Sandwich Hybridization Assay for HPV E2/E6 Gene Detection
This protocol outlines the development of an electrochemical DNA biosensor for the simultaneous detection of two genes, adapted from a study validating the method with clinical samples [40].
I. Research Reagent Solutions
Table 2: Essential Materials and Reagents
| Item | Function/Description |
|---|---|
| Screen-Printed Carbon Electrodes (SPCEs) | Disposable, portable electrochemical cell; working and counter electrodes are carbon, reference is Ag/AgCl. |
| Streptavidin Magnetic Beads | Solid support for the immobilization of biotinylated capture probes via strong streptavidin-biotin interaction. |
| Biotinylated Capture & Reporter Probes | Single-stranded DNA probes complementary to target sequences (E2, E6); capture probe immobilizes target, reporter probe enables detection. |
| Methylene Blue (MB) | A redox-active intercalator that binds preferentially to double-stranded DNA (hybridized product), serving as the electrochemical signal reporter. |
| Poly(allylamine hydrochloride) / Poly(sodium 4-styrenesulfonate) (PAA/PSS) | Polyelectrolytes used to form a multilayer film on magnetic beads, enhancing probe loading capacity and stability. |
| Hybridization Buffer | Typically a saline-sodium citrate (SSC) buffer with controlled pH and ionic strength to promote specific DNA hybridization. |
II. Step-by-Step Procedure
Capture Probe Immobilization:
- Functionalize streptavidin-coated magnetic beads with a PAA/PSS multilayer to increase surface area and binding sites.
- Incubate the functionalized beads with biotinylated capture probes specific for the E2 and E6 genes for 30 minutes at room temperature with gentle shaking.
- Use a magnetic rack to separate and wash the beads to remove unbound probes.
Sandwich Hybridization Assay:
- Incubate the probe-immobilized beads with the extracted DNA sample for 45 minutes. Target genes (E2, E6) will hybridize with their respective capture probes.
- Add biotinylated reporter probes to the mixture and incubate for another 45 minutes, forming a "capture probe-target-reporter probe" sandwich complex.
- Perform magnetic separation and washing steps stringently to eliminate non-specifically bound material.
Electrochemical Detection & Measurement:
- Re-suspend the final bead complex in an appropriate measurement buffer.
- Place a drop of the suspension onto the SPCE.
- Add Methylene Blue to the solution as a redox indicator.
- Apply a square wave voltammetry (SWV) potential scan. The measured reduction current of Methylene Blue is proportional to the amount of double-stranded DNA present, and thus to the concentration of the target gene.
- The E2/E6 ratio is calculated from the respective SWV peak currents to determine the physical state of the HPV-16 genome.
Protocol 2: AI-Assisted Deconvolution of Multiplexed Voltammetric Signals
This protocol describes a methodology for using machine learning to resolve overlapping signals in complex voltammograms, based on research using model quinone compounds [39].
I. Research Reagent Solutions
Table 3: Essential Materials and Reagents for AI-Assisted Analysis
| Item | Function/Description |
|---|---|
| Bare Screen-Printed Electrodes (SPEs) | Custom-made electrodes with graphite working and counter electrodes and an Ag/AgCl reference. |
| Standard Redox Probes | e.g., Ferrocyanide/Ferricyanide ([Fe(CN)₆]â´â»/³â»); provides a stable and well-understood reference signal for method validation. |
| Analyte Mixtures | Complex samples containing multiple electroactive species with similar redox potentials (e.g., hydroquinone, catechol). |
| Data Acquisition Software | e.g., PSTrace; controls the potentiostat and records voltammetric data. |
| Python/R Environment with ML Libraries | e.g., TensorFlow, Keras; for building, training, and deploying the deep learning model for signal classification and analysis. |
II. Step-by-Step Procedure
Data Acquisition & Pre-processing:
- Acquire voltammetric data (CV or SWV) for individual analytes and their mixtures across a range of concentrations and ratios.
- Perform all measurements in triplicate to ensure reproducibility.
- Format the voltammetric data (current vs. potential curves) into a structured dataset, normalizing the signals if necessary.
Data Transformation for ML:
- Convert the 1D voltammetric signals into 2D images using a transformation like the Gramian Angular Field (GAF). This encodes temporal correlation information into a graphical format that is well-suited for image-based deep learning models [39].
Model Training & Validation:
- Design a Convolutional Neural Network (CNN) architecture. A proposed structure includes multiple Conv2D and MaxPooling2D layers for feature extraction, followed by Flatten and Dense layers for classification [39].
- Split the dataset into training, validation, and test sets.
- Train the CNN model on the training set to classify the voltammetric images, identifying the presence and concentration of each analyte in the mixture.
- Validate the model's performance using the validation set, optimizing hyperparameters to prevent overfitting.
Deployment for Qualitative & Quantitative Analysis:
- Use the trained AI model to analyze new, unknown voltammetric data from complex samples.
- The model outputs the qualitative identification (classification) of the redox probes present and a semi-quantitative estimation of their concentrations, overcoming the limitations of manual peak assignment.
Workflow and Signaling Pathway Visualizations
Biosensor Fabrication and Detection Workflow
Diagram 1: Biosensor fabrication and detection workflow.
AI-Assisted Electrochemical Analysis Workflow
Diagram 2: AI-assisted electrochemical analysis workflow.
Integration with Microfluidics and System Automation for Sample-to-Answer Workflows
Within the field of cancer molecular diagnostics, the detection of gene fusions has emerged as a critical tool for diagnosis, prognosis, and guiding targeted therapies [13]. These hybrid genes, formed through chromosomal rearrangements such as translocations, deletions, or aberrant splicing, serve as vital molecular biomarkers [41]. The convergence of electrochemical (EC) biosensors with microfluidic automation creates powerful "sample-to-answer" systems that offer rapid, sensitive, and automated detection of these biomarkers, presenting a compelling alternative to traditional techniques like fluorescence in situ hybridization (FISH), polymerase chain reaction (PCR), and next-generation sequencing (NGS) [13] [41].
This document provides detailed application notes and protocols for developing and implementing such integrated systems, contextualized within broader research on electrochemical detection of fusion genes for cancer diagnosis.
System Components and Operational Principles
An automated sample-to-answer diagnostic system seamlessly integrates two core modules: a microfluidic platform for sample preparation and a biosensor module for detection and analysis [42].
Microfluidic Platform for Sample Preparation
The microfluidic component is responsible for the automated preparation of the biological sample, encompassing pathogen enrichment, nucleic acid (NA) extraction, and purification. The system utilizes a simple, low-cost disposable chip that can be easily fabricated and assembled [42].
- Pathogen Enrichment and NA Extraction: A key innovation involves using adipic acid dihydrazide (ADH), a homobifunctional hydrazide, for both pathogen enrichment and NA extraction. ADH selectively binds to negatively charged pathogens via electrostatic attraction. Subsequently, nucleic acids extracted from these pathogens bind to ADH through a combination of electrostatic attraction and covalent coupling, forming imine and hydrazone bonds [42].
- Fluidic Control: Automation is achieved by integrating syringe pumps (e.g., Hamilton 54848-01) to control solution volume and flow rate, manifolds (e.g., P-152) for fluid direction, and solenoid valves. This setup enables all sample preparation processes to be completed within 60 minutes in a single, automated workflow [42].
Electrochemical Detection Module
Electroanalytical methods provide a detection platform that is affordable, versatile, and portable without compromising specificity, sensitivity, or accuracy [13]. While the cited research details a bio-optical sensor, the principle of miniaturized, integrated detection aligns with the capabilities of electrochemical biosensors.
EC biosensors for fusion gene detection typically employ a solid-phase assay where a capture probe immobilized on an electrode surface hybridizes with a specific target sequence from the prepared sample. The hybridization event is transduced into a measurable electrical signal (e.g., change in current or impedance), allowing for quantitative analysis [13].
Application Notes: System Performance and Validation
The performance of an automated sample-to-answer system is rigorously validated through key parameters as summarized in the table below.
Table 1: Performance Metrics of an Automated Sample-to-Answer Diagnostic System
| Performance Parameter | Result / Specification | Methodology / Notes |
|---|---|---|
| Total Process Time | ~80 minutes [42] | 60 min for sample prep + 20 min for detection [42] |
| Limit of Detection (LOD) | 10x more sensitive than conventional methods [42] | Enabled by on-chip pathogen enrichment [42] |
| Analytical Sensitivity | 98.4% (62/63 known fusions detected) [43] | As demonstrated by a validated WTS assay [43] |
| Analytical Specificity | 100% (0 false positives in 21 negative samples) [43] | As demonstrated by a validated WTS assay [43] |
| Sample Input Volume | 1.0 - 2.5 mL [42] | System effectively concentrates pathogens across this range [42] |
| Sample Type Compatibility | Plasma, nasopharyngeal (NP) swabs, saliva [42] | Clinically validated for Q fever and COVID-19 detection [42] |
| RNA Quality Threshold | DV200 ≥ 30% [43] | Threshold for RNA degradation for reliable fusion detection [43] |
Clinical and Analytical Validation
The utility of integrated systems is proven through clinical validation. One system was successfully used to distinguish Q fever from other febrile diseases using 20 plasma samples and detected COVID-19 in 11 NP swabs and two saliva samples, demonstrating robust performance across different pathogens and sample matrices [42]. For gene fusion detection, establishing minimum RNA quality and quantity inputs is crucial; a validated whole transcriptome sequencing (WTS) assay defined optimal inputs as RNA greater than 100 ng and a minimum of 40 copies/ng for optimal sensitivity [43].
Detailed Experimental Protocols
Protocol 1: Microfluidic Nucleic Acid Extraction and Pathogen Enrichment
This protocol describes the procedure for automated NA extraction and pathogen enrichment using a ADH-functionalized microfluidic chip [42].
Research Reagent Solutions & Essential Materials: Table 2: Key Reagents and Materials for Microfluidic NA Extraction
| Item | Function / Description |
|---|---|
| Adipic Acid Dihydrazide (ADH) | Homobifunctional hydrazide for pathogen capture and NA binding [42]. |
| Microfluidic Chip | Disposable chip, often fabricated from PDMS or plastic, featuring integrated channels and chambers [42]. |
| RNeasy FFPE Kit (Qiagen) | For total RNA extraction from formalin-fixed paraffin-embedded (FFPE) samples prior to library prep [43]. |
| Lysis Buffer | Typically contains guanidinium isothiocyanate or SDS to lyse cells and inactivate nucleases. |
| Wash Buffers | Ethanol-based or low-salt buffers to remove impurities without eluting NAs. |
| Elution Buffer | Low-ionic-strength buffer (e.g., Tris-EDTA, nuclease-free water) for eluting purified NAs. |
Procedure:
- Chip Priming and Functionalization: Flush the microfluidic channels with a solution of ADH to coat the surface. Incubate to allow for stable immobilization.
- Sample Loading and Pathogen Enrichment: Introduce the raw or pre-processed sample (e.g., plasma, lysed tissue) into the chip. The flow rate is controlled by a syringe pump (e.g., 100 µL/min) to maximize contact time between the sample and the ADH-coated surface, facilitating pathogen capture via electrostatic interactions.
- Washing: Remove unbound cellular debris and contaminants by flowing a series of wash buffers through the chip.
- On-Chip Lysis: Introduce a lysis buffer to disrupt the captured pathogens and release intracellular nucleic acids. The released NAs subsequently bind to the ADH surface.
- Additional Washing: Perform a second wash series with a stringent buffer to remove proteins, salts, and other enzymatic inhibitors, leaving purified NAs bound to the chip.
- Elution: Elute the purified nucleic acids using a low-ionic-strength elution buffer. The eluate is now ready for downstream detection assays.
Protocol 2: Electrochemical Detection of Fusion Gene Transcripts
This protocol outlines the steps for detecting a specific fusion gene (e.g., EML4-ALK) using an electrochemical biosensor.
Research Reagent Solutions & Essential Materials: Table 3: Key Reagents and Materials for Electrochemical Detection
| Item | Function / Description |
|---|---|
| Capture Probe | Single-stranded DNA or RNA oligonucleotide complementary to a specific region of the target fusion sequence, modified with a thiol or amine group for electrode immobilization. |
| Electrochemical Reporter | Redox-active molecules (e.g., Methylene Blue, Ferrocene) or enzyme-based systems (e.g., Horseradish Peroxidase with Hâ‚‚Oâ‚‚/ TMB substrate). |
| Blocking Agent | Bovine Serum Albumin (BSA) or mercaptohexanol, used to block non-specific binding sites on the electrode surface. |
| Hybridization Buffer | A buffered saline solution (e.g., SSC buffer) with controlled pH and ionic strength to optimize hybridization kinetics and specificity. |
| Portable Potentiostat | Electronic instrument for applying potential and measuring the resulting current (e.g., for amperometry or DPV). |
Procedure:
- Electrode Functionalization: Immobilize thiolated capture probes onto a gold electrode surface via self-assembled monolayer formation. Alternatively, use carboxylated carbon electrodes with EDC/NHS chemistry to attach amine-modified probes.
- Surface Blocking: Incubate the functionalized electrode with a solution of BSA (1% w/v) or 6-mercapto-1-hexanol (1 mM) for 30-60 minutes to minimize non-specific adsorption.
- Hybridization: Introduce the extracted RNA or cDNA sample (from Protocol 1) to the electrode surface in a suitable hybridization buffer. Incubate for 15-30 minutes at a controlled temperature to allow for specific hybridization between the target fusion transcript and the immobilized capture probe.
- Signal Generation and Measurement:
- For a label-free approach: Measure the electrochemical impedance (EIS) in a solution containing [Fe(CN)₆]³â»/â´â». Hybridization increases interfacial resistance, leading to a measurable change in impedance.
- For a label-based approach: Incubate with a reporter probe conjugated to an electrochemical label (e.g., Horseradish Peroxidase). After washing, add an enzyme substrate (e.g., TMB/Hâ‚‚Oâ‚‚) and apply a specific potential to measure the generated amperometric current. The current is directly proportional to the amount of target present.
- Data Analysis: Quantify the target concentration by comparing the measured signal (current, impedance change) to a standard curve generated from known concentrations of synthetic target.
Visual Workflows and Signaling Pathways
The following diagrams, generated using DOT language, illustrate the core workflow of an integrated system and the oncogenic signaling pathway activated by a representative fusion gene.
Sample-to-Answer Workflow
EML4-ALK Signaling Pathway
Overcoming Key Challenges in Selectivity, Sensitivity, and Real-World Application
Mitigating Biofouling and Enhancing Selectivity in Complex Biological Matrices
The reliable electrochemical detection of specific fusion gene sequences in complex biological samples, such as serum or tumor lysates, is a cornerstone of modern cancer diagnostics and therapy monitoring [13] [14]. However, two significant and often intertwined challenges impede the accuracy and longevity of such biosensors: biofouling and insufficient selectivity. Biofouling, the nonspecific adsorption of proteins, cells, and other biomolecules onto sensor surfaces, can physically block analyte access, deteriorate sensor sensitivity, and trigger a foreign body response that leads to fibrous encapsulation and eventual sensor failure [44] [45]. Simultaneously, achieving high selectivity to distinguish target fusion gene sequences from a background of analogous nucleic acids, proteins, and other matrix components is paramount for a clinically meaningful result [14]. This Application Note details practical protocols and strategies to mitigate biofouling and enhance selectivity, enabling robust electrochemical detection of fusion genes for cancer research.
Background
The Impact of Biofouling on Electrochemical Sensors
Upon implantation or exposure to biological fluids, electrochemical sensors immediately encounter a complex environment that can compromise their function. The spontaneous accumulation of biomolecules (e.g., proteins, lipids) and cells on the sensor surface is known as biofouling [44]. For electrochemical probes, this fouling layer manifests as an increase in electrochemical impedance, a shift in the background signal, and diminished sensitivity and selectivity to the target analyte [45]. In long-term fast-scan cyclic voltammetry (FSCV) studies, for example, biofouling causes a cathodic polarization of the Ag/AgCl reference electrode and increases the impedance of both the reference and working electrodes, directly impacting the quality of neurotransmitter detection [45]. These events are primarily driven by the immune system's foreign body response to the implanted device, leading to encapsulation [44] [45].
The Necessity of Selectivity in Fusion Gene Detection
Fusion genes, formed by the joining of two separate genes, are critical diagnostic and prognostic biomarkers in hematological malignancies and solid tumors [13]. Electrochemical biosensors offer a promising route for their detection due to their speed, cost-effectiveness, and sensitivity [14]. However, the clinical sample matrix (e.g., blood, plasma) contains a multitude of interferents that can generate false-positive or false-negative signals. Therefore, the biosensor must be designed to transduce only the specific target fusion gene sequence with high fidelity, necessitating a multi-layered approach to selectivity that encompasses biorecognition, surface chemistry, and electrochemical techniques [14] [44].
Anti-Biofouling Strategies and Protocols
Anti-biofouling strategies can be broadly classified into passive (creating surfaces that resist adhesion) and active (disrupting or removing the fouling layer) approaches. The following table summarizes the most promising materials and methods.
Table 1: Overview of Anti-Biofouling Strategies for Electrochemical Biosensors
| Strategy Type | Specific Material/Method | Mechanism of Action | Key Advantages | Potential Limitations |
|---|---|---|---|---|
| Passive | Zwitterionic Polymers (e.g., poly(carboxybetaine)) | Forms a hydration layer via electrostatic interactions, creating a physical and energetic barrier to biomolecule adsorption [44]. | Highly effective resistance to non-specific protein adsorption; excellent biocompatibility. | Can require complex surface conjugation chemistry. |
| Passive | Poly(ethylene glycol) (PEG) and Hydrophilic Polymers | Creates a steric hindrance and hydrated surface that is energetically unfavorable for protein adhesion [44]. | Well-established, commercially available reagents. | Susceptible to oxidative degradation in vivo. |
| Passive | Slippery Liquid-Infused Porous Surfaces (SLIPS/SNIPS) | A lubricating fluid locked in a porous substrate creates a smooth, dynamically reparable surface that repels biological fluids and cells [46]. | Excellent repellency to broad spectrum of foulants (blood, bacteria); physical damage can be healed. | Long-term stability of the lubricant layer under flow conditions. |
| Active | Nitric Oxide (NO)-Releasing Materials (e.g., GSNO) | Localized release of NO, a bioactive molecule with inherent antibacterial and anti-platelet properties, prevents biofilm formation and thrombosis [46]. | Potent antibacterial and anti-platelet action; mimics endothelial function. | Finite NO release duration; requires stabilization of NO donors. |
| Active | Electrochemical Impedance Compensation | Using a three-electrode system designed to compensate for fouling-induced impedance changes [45]. | Preserves sensor sensitivity and selectivity; addresses an electrochemical consequence of fouling. | Does not prevent the fouling accumulation itself. |
| Active | Mechanical Actuation | Physical movement or vibration of the sensor to dislodge adhered biofilms [44]. | Can effectively remove established fouling layers. | Increases system complexity and power requirements. |
Protocol: Fabrication of a Zwitterionic Polymer-Coated Electrode
This protocol details the modification of a gold disk electrode with a poly(carboxybetaine) (pCB) brush layer to minimize non-specific adsorption.
Materials:
- Gold disk working electrode (2 mm diameter)
- Carboxybetaine acrylamide (CBAA) monomer
- 11-Mercapto-1-undecanol (MU)
- 2-Bromoisobutyryl bromide (BiB)
- Triethylamine (TEA)
- Copper(II) Bromide (CuBrâ‚‚), Copper(I) Bromide (CuBr), and 2,2'-Bipyridyl (Bpy) for ATRP
- Absolute Ethanol, Deionized (DI) Water, Phosphate Buffered Saline (PBS, pH 7.4)
- Nitrogen gas
Equipment:
- Potentiostat/Galvanostat
- Ultrasonic cleaner
- Oxygen-free glove box or Schlenk line
Procedure:
- Electrode Pretreatment: Clean the gold electrode by polishing with 0.05 μm alumina slurry on a microcloth, followed by sequential sonication in ethanol and DI water for 5 minutes each. Electrochemically clean by performing cyclic voltammetry (CV) in 0.5 M H₂SO₄ from -0.2 to 1.5 V (vs. Ag/AgCl) until a stable CV profile is obtained. Rinse thoroughly with DI water and dry under N₂ stream.
- Self-Assembled Monolayer (SAM) Formation: Immerse the clean electrode in a 1 mM ethanolic solution of 11-mercapto-1-undecanol (MU) for 16-24 hours at room temperature in the dark. This forms a hydroxyl-terminated SAM.
- ATRP Initiator Immobilization: Rinse the MU-modified electrode with ethanol and dry under N₂. Transfer to a dry glass vial containing 10 mL of anhydrous dichloromethane. Add 100 μL of TEA and 50 μL of 2-bromoisobutyryl bromide (BiB) to the solution. React for 30 minutes with gentle stirring to esterify the terminal hydroxyl groups, immobilizing the ATRP initiator. Rinse thoroughly with dichloromethane and ethanol.
- Surface-Initiated ATRP of CBAA: Prepare the polymerization solution in a Schlenk flask: dissolve 2 g of CBAA monomer and 100 mg of Bpy in 20 mL of a 1:1 (v/v) methanol/water mixture. Degas with Nâ‚‚ for 30 minutes. Add 15 mg of CuBr and 5 mg of CuBrâ‚‚ under a Nâ‚‚ atmosphere. Transfer the initiator-modified electrode to the flask and seal. Allow the polymerization to proceed for 1-2 hours at room temperature.
- Termination and Cleaning: Remove the electrode from the polymerization solution and immerse it in DI water to terminate the reaction. Soak the electrode in PBS for 24 hours with frequent buffer changes to remove any unreacted monomer and copper catalyst.
- Validation: Characterize the modified electrode using electrochemical impedance spectroscopy (EIS) in a solution containing 5 mM K₃[Fe(CN)₆]/K₄[Fe(CN)₆] in PBS. A successful pCB modification will show a significant increase in charge-transfer resistance (Rₑₜ) due to the hydrated, non-conductive polymer brush. Test anti-fouling performance by incubating the electrode in 10% fetal bovine serum (FBS) for 1 hour and re-measuring EIS; the Rₑₜ should show minimal change compared to a bare gold electrode.
Protocol: Integrating a Slippery Nanoemulsion (SNIPS) Coating
This protocol describes creating a dual-action, slippery, and nitric oxide (NO)-releasing surface on a porous polymer substrate, which could be used as a sensor membrane or housing.
Materials:
- Expanded Polytetrafluoroethylene (ePTFE) membrane (or other porous polymer).
- S-Nitrosoglutathione (GSNO): Synthesized as per [46] from reduced glutathione and sodium nitrite.
- Span 80 (sorbitan monooleate), Tween 80 (polyoxyethylene (20) sorbitan monooleate).
- n-Hexadecane.
- Phosphate Buffered Saline (PBS) with 100 μM EDTA.
Equipment:
- Sonicator (with probe tip).
- Magnetic stirrer.
- NO Analyzer (for calibration and validation).
Procedure:
- GSNO-Nanoemulsion (NE) Preparation: Dissolve GSNO (e.g., 50 mM) in PBS with 100 μM EDTA (aqueous phase). In a separate vial, prepare the oil phase by mixing Span 80 and n-hexadecane (e.g., 4:96 w/w). Slowly add the oil phase to the aqueous phase under low-energy magnetic stirring to form a coarse emulsion. Subsequently, subject the mixture to high-energy probe sonication (e.g., 40% amplitude for 2-3 minutes in an ice bath) to form a stable water-in-oil (w/o) nanoemulsion.
- Substrate Infusion: Drop-cast the prepared GSNO-NE onto the ePTFE membrane until the surface appears glossy and saturated. Allow the infused membrane to rest for 1 hour to stabilize.
- Characterization:
- Slipperiness: Measure the sliding angle for a water droplet (e.g., 10 μL). A sliding angle of <10° indicates successful infusion.
- NO Release: Quantify the NO release profile over 24-48 hours using a chemiluminescence NO analyzer. The material should release NO at physiological levels (e.g., 0.5 - 4 × 10â»Â¹â° mol cmâ»Â² minâ»Â¹) [46].
- Antibacterial Adhesion: Perform a 4-hour bacterial adhesion assay with S. aureus and E. coli. The SNIPS-coated substrate should show a >90% reduction in bacterial adhesion compared to unmodified control [46].
Enhancing Selectivity: Materials and Methods
Enhancing selectivity requires a multi-faceted approach combining specific biorecognition elements, permselective membranes, and advanced electrochemical techniques.
Table 2: Strategies for Enhancing Selectivity in Complex Matrices
| Strategy Layer | Method | Principle | Application Note |
|---|---|---|---|
| Biorecognition | Locked Nucleic Acid (LNA) Probes | LNA nucleotides bind complementary DNA/RNA with exceptionally high affinity and specificity, improving single-nucleotide polymorphism (SNP) discrimination [14]. | Ideal for designing probes against the unique junction sequence of fusion genes. |
| Signal Transduction | Redox Labels (e.g., Methylene Blue, Ferrocene) | Using a specific redox reporter attached to the signaling probe moves the detection signal to a potential window with less interference from endogenous electroactive species [14]. | Reduces background current from ascorbic acid, uric acid, etc. |
| Surface Barrier | Nafion Membranes | A permeslective, cation-exchange coating repels negatively charged interferents like uric acid and DNA/RNA fragments, while allowing small neutral species (e.g., Hâ‚‚Oâ‚‚) to pass [44]. | Highly effective when coupled with enzyme-based (e.g., HRP) detection schemes. |
| Data Acquisition | Multiple Reaction Monitoring (MRM³) | An LC-MS/MS technique that provides an added layer of specificity by performing two sequential fragmentation steps, virtually eliminating background interference [47]. | While an MS technique, its principle inspires the use of multi-level verification in electrochemical assays. |
Protocol: Designing a Selective LNA-Based Sandwich Assay with a Nafion Barrier
This protocol outlines the development of an electrochemical DNA sensor (genosensor) for a specific fusion gene (e.g., BCR-ABL) using a sandwich hybridization approach with LNA capture probes and a Nafion-coated electrode.
Materials:
- LNA Capture Probe: Thiol-modified LNA probe complementary to a segment of the fusion gene.
- LNA Signaling Probe: Bioinylated LNA probe complementary to an adjacent segment of the fusion gene.
- Streptavidin-Conjugated Horseradish Peroxidase (SA-HRP)
- Hydrogen Peroxide (Hâ‚‚Oâ‚‚)
- TMB Substrate (or Hydroquinone)
- Nafion (5% w/w solution)
- Gold or Screen-Printed Carbon Electrode (SPCE)
Procedure:
- Electrode Modification with Nafion: Dilute the 5% Nafion stock solution to 0.5-1% in ethanol. Drop-cast 5 μL of this solution onto the cleaned SPCE and allow it to dry at room temperature for 1 hour. This forms a thin, permselective film.
- Immobilization of LNA Capture Probe: Incubate the Nafion-coated electrode with a 1 μM solution of the thiolated LNA capture probe in immobilization buffer (e.g., PBS with 1 M MgCl₂) for 1 hour. The thiol group will covalently bind to the gold surface (if using SPCE, pre-modify with Au nanoparticles or use avidin-biotin chemistry). Rinse to remove unbound probes.
- Sandwich Hybridization:
- Step 1: Incubate the probe-modified electrode with the sample solution containing the target fusion gene RNA for 30 minutes at a controlled temperature (e.g., 40°C). Wash stringently.
- Step 2: Incubate the electrode with a solution containing the biotinylated LNA signaling probe for 30 minutes. Wash stringently.
- Step 3: Incubate the electrode with a solution of SA-HRP for 15 minutes. Wash thoroughly.
- Electrochemical Detection: Transfer the electrode to an electrochemical cell containing a suitable HRP substrate (e.g., Hâ‚‚Oâ‚‚ and hydroquinone). Measure the amperometric current generated by the reduction of benzoquinone (the oxidized product of hydroquinone) at a low applied potential (e.g., -0.2 V vs. Ag/AgCl). The current is directly proportional to the amount of captured fusion gene RNA.
The workflow for this multi-layered strategy, integrating both anti-biofouling and selectivity-enhancing components, is summarized in the following diagram:
Diagram 1: Integrated workflow for fabricating a robust biosensor combining anti-biofouling (green) and selectivity-enhancing (red) strategies.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Biofouling and Selectivity Research
| Reagent/Material | Function | Example Application | Key Consideration |
|---|---|---|---|
| Carboxybetaine Acrylamide (CBAA) | Monomer for grafting zwitterionic polymer brushes onto sensor surfaces [44]. | Creating ultra-low fouling gold electrode surfaces for direct detection in serum. | Requires controlled polymerization techniques like ATRP. |
| S-Nitrosoglutathione (GSNO) | Nitric oxide (NO) donor for fabricating active anti-biofouling materials [46]. | Loading into nanoemulsions to create NO-releasing sensor membranes or coatings. | Light and temperature-sensitive; requires synthesis and storage in the dark. |
| Locked Nucleic Acid (LNA) Probes | High-affinity nucleic acid analogs for biorecognition, offering superior specificity and duplex stability [14]. | 用作æ•èŽ·å’Œä¿¡å·æŽ¢é’ˆï¼Œç”¨äºŽæ£€æµ‹èžåˆåŸºå› 的夹心æ‚交测定。 | 相对于DNA/RNA探针,æˆæœ¬æ›´é«˜ï¼›éœ€è¦ä»”细设计以é¿å…自退ç«ã€‚ |
| Nafion Perfluorinated Resin | Cation-exchange polymer used as a permselective membrane to repel anionic interferents [44]. | Coating on carbon electrodes to reduce fouling from serum proteins and uric acid in amperometric detection. | Optimal dilution and casting volume are critical to avoid hindering analyte diffusion. |
| Span 80 / Tween 80 Surfactants | Non-ionic surfactants for stabilizing water-in-oil nanoemulsions [46]. | Forming the oil continuous phase for SNIPS coatings on sensor materials. | The HLB value determines the emulsion type (w/o vs. o/w). |
| Rifaquizinone | Rifaquizinone, CAS:922717-97-3, MF:C65H81FN6O15, MW:1205.4 g/mol | Chemical Reagent | Bench Chemicals |
| CCT-251921 | CCT-251921, CAS:1607837-31-9, MF:C21H23ClN6O, MW:410.906 | Chemical Reagent | Bench Chemicals |
The path to reliable electrochemical detection of fusion genes in real-world samples is paved with the challenges of biofouling and matrix interference. By systematically implementing the strategies and protocols outlined in this Application Note—ranging from the grafting of zwitterionic polymers and the application of SLIPS/SNIPS coatings for fouling mitigation, to the use of LNA probes and permselective membranes for enhanced selectivity—researchers can significantly improve the accuracy, longevity, and clinical utility of their biosensing platforms. The integration of these passive and active methods into a cohesive sensor design, as visualized in the workflows, provides a robust framework for advancing cancer diagnosis and monitoring through electrochemical fusion gene detection.
Addressing Biomarker Heterogeneity and Variability through Multipiplexed Sensor Arrays
The inherent heterogeneity of cancer biomarkers presents a significant challenge for precise diagnosis and prognostic monitoring. Single-analyte detection methods often fail to capture the complex molecular "fingerprints" indicative of disease state and progression. Multiplexed sensor arrays represent a transformative technological solution, enabling the simultaneous measurement of multiple biomarker targets from a single sample. This approach is particularly valuable in the context of electrochemical detection of fusion genes, where parallel assessment of genetic markers can provide critical insights into cancer pathogenesis and therapeutic response. By addressing biomarker variability comprehensively, these platforms pave the way for more personalized and effective cancer diagnostics [48].
The Rationale for Multiplexed Detection
Limitations of Single-Analyte Approaches
Traditional single-analyte detection methods, such as conventional ELISA, provide limited biological context when faced with disease heterogeneity. In cancer, individual biomarkers may be elevated in only a subset of patients or may correlate differently with disease progression across patient populations. For example, in cervical cancer associated with human papillomavirus type 16 (HPV-16), the physical state of the viral genome (episomal versus integrated) represents a critical diagnostic parameter that requires simultaneous detection of both E2 and E6 genes for accurate assessment [40]. Similarly, in chronic myeloid leukemia, detection of the BCR/ABL fusion gene fragment requires highly specific recognition to distinguish it from similar genetic sequences [49].
Advantages of Multiplexed Sensor Arrays
Multiplexed arrays address variability by capturing biomarker panels that provide organ-specific or disease-specific signatures. Research has demonstrated that selected patient samples reveal unique biomarker "fingerprints" with potential utility for personalized cancer diagnosis [48]. Silicon photonic microring resonator technology, for instance, has successfully simultaneously detected eight cancer biomarkers applicable to pancreatic, liver, ovarian, breast, lung, colorectal, and prostate cancers, including α-fetoprotein (AFP), cancer antigen 15-3 (CA15-3), cancer antigen 19-9 (CA19-9), cancer antigen-125 (CA-125), carcinoembryonic antigen (CEA), osteopontin, and prostate specific antigen (PSA) [48].
Multiplexed Sensor Platforms and Methodologies
Silicon Photonic Microring Resonators
Silicon photonic microring resonators belong to the class of refractive index-responsive "whispering gallery resonators" that leverage semiconductor fabrication methods to create multiplexable sensor arrays. These sensors operate on the principle of optical resonance, where binding-induced changes in the local refractive index at the sensor surface quantitate the presence of target analytes [48].
Operating Principle: Light couples into microring resonators from adjacent linear waveguides under conditions of optical resonance, described by: [ m\lambda = 2\pi n{\text{eff}} ] where ( m ) is an integer, ( \lambda ) is the wavelength of light, ( r ) is the radius of the ring, and ( n{\text{eff}} ) is the effective refractive index of the waveguide mode [48].
Array Configuration: Experiments utilizing the Maverick M1 instrumentation employ sensor chips with 32 active microring sensors, with two additional sensors used to correct for thermal drift. This configuration enables detection of eight different analytes, each measured in quadruplicate, facilitating robust statistical analysis [48].
Electrochemical Biosensors
Electrochemical biosensors offer an alternative platform for multiplexed detection with advantages of simplicity, fast response, and low cost. These sensors have been applied to fusion gene detection, such as BCR/ABL in chronic myeloid leukemia and E2/E6 genes in HPV-16 [49] [40].
Signal Amplification Strategies: To overcome limitations of inadequate sensitivity and specificity, electrochemical platforms employ sophisticated signal amplification strategies:
- Polymerase-Assisted Multiplication: Circular strand displacement polymerization (CSRP) assisted by polymerase enables target duplication without requiring specific recognition sites [49].
- Quantum Dot Tagging: Massively parallel signal labels such as quantum dots provide enhanced detection sensitivity through anodic stripping voltammetry (ASV) [49].
- Cascade Hybridization: Primer-mediated cascade hybridization generates long double helices that offer numerous active sites for signal label loading [49].
Table 1: Performance Comparison of Multiplexed Sensor Platforms
| Platform | Detection Method | Multiplexing Capacity | Sensitivity | Assay Time | Key Applications |
|---|---|---|---|---|---|
| Silicon Photonic Microring Resonators | Optical resonance shift | 8-plex demonstrated (32 sensors total) | Clinically relevant levels with signal enhancement | ~90 minutes | Protein cancer biomarkers (AFP, CA15-3, CA19-9, CA-125, CEA, osteopontin, PSA) |
| Electrochemical DNA Biosensor | Anodic stripping voltammetry | Duplex (E2/E6 genes) | 8-12 copies/mL | Rapid (specific time not stated) | HPV-16 E2/E6 fusion genes, BCR/ABL fusion gene |
Experimental Protocols
Silicon Photonic Array for Protein Biomarker Detection
Sensor Functionalization
- Antibody Immobilization: Employ DNA-encoded antibody method for robust, on-demand antibody array creation [48].
- Surface Chemistry: Functionalize microring resonators with target-specific capture antibodies via appropriate crosslinking chemistry.
- Quality Control: Validate antibody immobilization through real-time resonance wavelength monitoring.
Sample Processing and Assay
- Sample Preparation: Dilute serum samples in appropriate running buffer to minimize matrix effects.
- Primary Binding: Flow sample across pre-functionalized microring resonator array for 30 minutes to allow antigen binding to capture antibodies.
- Rinsing Phase: Switch to running buffer for 20 minutes to remove unbound material.
- Sandwich Complex Formation: Introduce biotinylated tracer antibodies to form complete immunocomplex.
- Signal Enhancement:
- Introduce PE-labeled anti-biotin antibodies which bind to biotinylated tracer antibodies.
- Add biotinylated anti-PE antibodies which bind to PE labels.
- Repeat cycles (typically 3 cycles maximum) to exponentially amplify signal [48].
- Real-time Monitoring: Observe resonance wavelength shifts throughout all assay steps using the Maverick M1 automated instrumentation.
Electrochemical Duplex Detection of Fusion Genes
Probe Design and Immobilization
- Oligonucleotide Design: Design capture probes, reporter probes, and blocking probes based on target gene sequences (e.g., E2 and E6 genes of HPV-16) [40].
- Surface Preparation: Immobilize thiolated molecular beacons on electrode surface through Au-thiol bond formation [49].
- Capture Probe Attachment: Functionalize magnetic beads with biotinylated capture probes and blocking probes using streptavidin-biotin chemistry [40].
Target Amplification and Detection
- Target Recognition: Hybridize target sequence to molecular beacons, opening the stem-loop structure and exposing the stem sequence [49].
- Circular Strand Displacement Polymerization: In the presence of Klenow Fragment (3' → 5' exo-), initiate CSRP to generate numerous primer sequences [49].
- Cascade Hybridization: Allow generated primers to trigger formation of long double helices through hybridization with amplification probes [49].
- Quantum Dot Tagging: Load cadmium sulfide (CdS) and zinc sulfide (ZnS) quantum dots onto the formed double helices [49].
- Electrochemical Measurement: Perform anodic stripping voltammetry to detect dissolved metal ions from quantum dots, with peak currents proportional to target concentration [49].
Data Quality Assurance and Analysis
Quantitative Data Quality Assurance
Effective quality assurance procedures are essential for reliable multiplexed sensor data:
- Data Cleaning: Identify and remove duplicate measurements and questionnaires with certain thresholds of missing data [50].
- Anomaly Detection: Check data for deviations from expected patterns using descriptive statistics [50].
- Missing Data Management: Use Little's Missing Completely at Random (MCAR) test to determine pattern of missingness and apply appropriate imputation methods if needed [50].
- Psychometric Validation: Establish reliability and validity of measurement instruments, with Cronbach's alpha scores >0.7 considered acceptable for internal consistency [50].
Statistical Analysis Approaches
- Normality Testing: Assess data distribution using kurtosis, skewness, Kolmogorov-Smirnov, or Shapiro-Wilk tests before selecting appropriate statistical tests [50].
- Descriptive Statistics: Calculate frequencies, means, medians, modes, and standard deviations to summarize dataset characteristics [51].
- Inferential Analysis: Employ parametric or non-parametric tests based on data distribution characteristics to compare groups, analyze relationships, or make predictions [50].
Table 2: Research Reagent Solutions for Multiplexed Sensor Applications
| Reagent/Material | Function | Application Examples | Specific Implementation |
|---|---|---|---|
| Silicon Photonic Sensor Chips | Transduction platform for optical detection | Protein cancer biomarker panels | 32-microring arrays with thermal drift correction [48] |
| Screen-Printed Carbon Electrodes (SPCE) | Disposable electrode platform for electrochemical detection | Fusion gene detection | Two-electrode systems for HPV-16 E2/E6 detection [40] |
| DNA-Encoded Antibodies | Capture agent for specific antigen recognition | Multiplexed protein detection | Enables robust antibody array creation [48] |
| Molecular Beacons | Structured nucleic acid probes for target recognition | Fusion gene detection | Thiol-modified for electrode immobilization [49] |
| Quantum Dots (CdS, ZnS) | Signal amplification labels | Ultrasensitive electrochemical detection | Metal ions measured via anodic stripping voltammetry [49] |
| Streptavidin Magnetic Beads | Solid support for probe immobilization | Nucleic acid target capture | Facilitates separation and concentration [40] |
| Klenow Fragment (3' → 5' exo-) | DNA polymerase for amplification | Circular strand displacement polymerization | Generates numerous primers from target [49] |
| Poly(allylamine hydrochloride) (PAA) | Surface modification polymer | Electrode functionalization | Improves probe immobilization efficiency [40] |
Experimental Workflows and Signaling Pathways
Workflow for Multiplexed Protein Biomarker Detection
Multiplexed Protein Detection Workflow: This diagram illustrates the automated protocol for detecting multiple protein biomarkers simultaneously using silicon photonic microring resonators, highlighting key steps including sensor functionalization, sample application, and signal enhancement [48].
Electrochemical Fusion Gene Detection Mechanism
Fusion Gene Detection Mechanism: This workflow details the electrochemical biosensing approach for fusion gene detection, featuring signal amplification through circular strand displacement polymerization and quantum dot tagging [49].
HPV-16 Physical State Determination Logic
HPV-16 Physical State Logic: This decision pathway illustrates how simultaneous detection of E2 and E6 genes with ratio analysis discriminates between episomal and integrated forms of HPV-16, providing critical diagnostic information for cervical cancer risk assessment [40].
Multiplexed sensor arrays represent a powerful approach to addressing the challenges of biomarker heterogeneity and variability in cancer diagnostics. By enabling simultaneous detection of multiple biomarkers—whether proteins or fusion genes—these platforms provide comprehensive molecular profiles that enhance diagnostic accuracy and enable personalized assessment. The experimental protocols and quality assurance measures outlined in this application note provide researchers with practical frameworks for implementing these advanced detection methodologies. As multiplexing technologies continue to evolve, their integration into clinical practice promises to transform cancer diagnosis, monitoring, and therapeutic decision-making.
Strategies for Long-Term Stability, Reproducibility, and Biocompatibility of Sensors
The electrochemical detection of fusion genes represents a transformative approach in cancer diagnostics, offering the potential for rapid, specific, and point-of-care identification of oncogenic biomarkers such as BCR-ABL, EML4-ALK, and NTRK fusions [52] [13]. Unlike traditional determination techniques, electroanalytical technologies provide affordable, versatile, and portable methods without compromising specificity, sensitivity, or accuracy [13]. However, the translation of these biosensors from research tools to reliable clinical platforms depends on addressing three interconnected fundamental challenges: ensuring long-term stability for continuous monitoring, maintaining reproducibility across manufacturing batches and operational conditions, and achieving biological compatibility for complex sample matrices.
This application note details practical strategies and standardized protocols to overcome these critical limitations. By integrating advances in interface engineering, material science, and quality control procedures, researchers can develop robust sensing systems capable of supporting the demanding requirements of cancer diagnosis, therapeutic monitoring, and personalized treatment strategies.
Core Challenges in Sensor Development
Long-Term Stability Limitations
Nucleic acid-based electrochemical sensors (NBEs) face significant stability challenges that preclude their long-term deployment. The most common limitation involves the desorption of thiol-based monolayers from gold electrode surfaces when exposed to environmental factors such as dry air, high temperatures, voltage pulsing, and biological fluids [53]. This desorption process simultaneously removes both sensing moieties and passivating thiols, typically limiting sensor deployment to a few hours [53]. Additionally, biofouling in serum or blood leads to protein deposition on the sensor interface, restricting the conformational dynamics of electrode-attached nucleic acids and reducing electron transfer efficiency [53]. Continuous in-vivo measurements using electrochemical aptamer-based sensors, for instance, have only been demonstrated for approximately 12 hours to date due to these limitations [53].
Reproducibility Concerns
Sensor-to-sensor and batch-to-batch variability presents a major obstacle for clinical adoption. Reproducibility issues stem from inconsistent fabrication processes, electrode surface heterogeneity, and variable probe immobilization efficiency. Furthermore, signal degradation over time, driven by processes such as the loss of antibodies and the dissociation of analogue molecules from the sensor surface, leads to reduced sensor sensitivity and selectivity during continuous operation [54]. This gradual performance shift complicates calibration and data interpretation across different devices and timepoints.
Biocompatibility Requirements
For sensors operating in biological environments, biocompatibility encompasses both mechanical compatibility with tissues and immunity to biofouling. The host response to implanted sensors typically involves protein adsorption and subsequent cell adhesion, culminating in the isolation of the implant by thrombi or scar tissue [55]. This cellular presence alters analyte transport in the region surrounding the sensor, compromising accuracy and usable lifetime. As such, "analytical biocompatibility" must describe improvements to in-vivo sensor performance directed specifically at reducing this host response [55].
Table 1: Key Performance Challenges and Their Impact on Sensor Function
| Challenge | Primary Causes | Impact on Sensor Performance |
|---|---|---|
| Monolayer Instability | Desorption of thiol-based monolayers from gold surfaces [53] | Limited operational lifetime (typically hours); signal drift |
| Biofouling | Non-specific protein adsorption in biological fluids [53] [55] | Reduced signal gain; hindered electron transfer; false positives/negatives |
| Signal Degradation | Loss of capture probes or binding agents over time [54] | Decreased sensitivity and selectivity; requires frequent recalibration |
| Host Immune Response | Foreign body reaction to implanted sensors [55] | Formation of fibrotic capsule; altered analyte transport; inaccurate readings |
Engineering Strategies for Enhanced Performance
Strategies for Long-Term Stability
Advanced Monolayer Chemistries: Replacing traditional monodentate thiols (e.g., 6-mercapto-hexanol) with multidentate anchoring groups significantly enhances monolayer stability through the chelate effect. Flexible trithiol anchors have demonstrated 94% signal retention after 50 electrochemical scans compared to ~75% for monothiols [53]. Post-deposition crosslinking strategies using agents like 1,11-bis-maleimidotriethyleneglycol (BM(PEG)3) can further improve stability, with crosslinked sensors retaining >90% hybridization capacity after 3 hours at 90°C, where monothiol sensors show undetectable capacity [53]. Additionally, employing hydrophobic thiols (e.g., hexanethiol) instead of hydrophilic counterparts increases packing density and reduces solubility, enabling signal retention for more than 80 hours in buffered solutions [53].
Anti-Biofouling Interfaces: Zwitterionic monolayers create a hydration barrier that resists non-specific protein adsorption, while hydrogel coatings provide a physiologically compatible interface that minimizes fouling [53]. For implantable applications, nanoporous gold electrodes can exclude proteins and cells based on size, allowing target analytes to diffuse into pores while restricting larger fouling agents [53].
Redox Reporter and Interrogation Optimization: Moving beyond the commonly used methylene blue—which has negative reduction potential overlapping with oxygen reduction and pH-dependent signaling—can improve stability [53]. Similarly, alternative electrochemical interrogation methods to square-wave voltammetry (SWV), whose voltage pulsing can accelerate monolayer desorption, should be explored to balance signal intensity with operational lifetime [53].
Ensuring Reproducibility
Standardized Fabrication Protocols: Implementing rigorous cleaning protocols for electrode surfaces prior to functionalization is essential. This includes chemical treatment, electrochemical activation, and plasma cleaning to ensure consistent starting surfaces. Automated microfluidic systems like the LSPone programmable syringe pump enable precise fluid handling with low internal volume (as low as 3.5 µL) and minimal carryover (1.5-10.2 µL), ensuring consistent reagent delivery and washing steps during sensor fabrication and operation [54].
Quality Control Metrics: Establishing pre-deployment calibration checks for each sensor batch using standardized control samples verifies functionality. Monitoring key fabrication parameters such as monolayer coverage via electrochemical impedance spectroscopy (EIS) ensures consistency. AI-driven optimization can significantly enhance reproducibility metrics, reducing false positives/negatives from 15-20% to 5-10% and improving calibration accuracy to a <2% margin of error compared to 5-10% with conventional methods [56].
Stability-Enhancing Formulations: Integrating stability agents directly into sensing formulations, such as adding antioxidants to reduce redox reporter degradation or using crowding agents to maintain probe activity, can improve lot-to-lot consistency.
Table 2: Quantitative Performance Improvements with AI-Optimized Aptasensors
| Performance Parameter | Ordinary Aptasensors | AI-Optimized Aptasensors |
|---|---|---|
| Sensitivity | 60 - 75% | 85 - 95% [56] |
| Specificity | 70 - 80% | 90 - 98% [56] |
| False Positive/Negative Rate | 15 - 20% | 5 - 10% [56] |
| Response Time | 10 - 15 seconds | 2 - 3 seconds [56] |
| Data Processing Speed | 10 - 20 minutes per sample | 2 - 5 minutes per sample [56] |
| Detection Limit (Examples) | -- | CEA: 10 fM (EIS); MUC1: 20 fM (EIS); PSA: 1 pM (DPV) [56] |
Achieving Biocompatibility
Mechanical Biocompatibility: For wearable and implantable sensors, mechanical compatibility with biological tissues is essential. This can be achieved through structural engineering strategies including "island-bridge" layouts, where conductive wires (bridges) interconnect rigid functional components (islands), as well as serpentine structures that convert rigid materials into stretchable configurations [57]. Implementing thin layer designs according to Euler-Bernoulli beam theory allows bending to small radii of curvature without fracture [57]. Additionally, using flexible materials with elastic moduli similar to skin, such as PDMS, polyvinyl alcohol (PVA), or polyethene terephthalate (PET), ensures optimal skin-device contact and adhesion [57].
Immune Biocompatibility: Natural biomaterials such as chitosan and pollen offer superior biological characteristics including renewability, low cost, biodegradability, and self-adherence, making them more skin-friendly for long-term deployment [57]. These materials exhibit low toxicity and do not cause inflammation on the skin surface, which is critical for extended monitoring applications limited by the natural turnover cycle of epithelial cells (approximately two weeks) [57].
Surface Modification Strategies: Crafting surfaces with non-biofouling polymers such as polyethylene glycol (PEG) or zwitterionic compounds reduces protein adsorption. For implantable applications, creating biomimetic surfaces that resemble natural cell membranes can trick the immune system into tolerating the device.
Application Notes for Fusion Gene Detection
Experimental Protocol: Fabrication of Stable E-AB Fusion Gene Sensors
Materials Required:
- Gold working electrodes (2 mm diameter)
- Thiolated DNA probes specific to target fusion gene (e.g., BCR-ABL)
- Flexible trithiol anchoring compound (e.g., THIOTRIS, Sigma-Aldrich 711420)
- Hydrophobic passivation thiol (e.g., hexanethiol)
- BM(PEG)3 crosslinker
- Electrochemical cell with Ag/AgCl reference and Pt counter electrodes
- LSPone or equivalent programmable syringe pump system [54]
- Potentiostat with impedance capabilities
Step-by-Step Procedure:
Electrode Pretreatment:
- Clean gold electrodes via chemical etching in piranha solution (3:1 Hâ‚‚SOâ‚„:Hâ‚‚Oâ‚‚) for 1 minute (caution: highly exothermic).
- Rinse thoroughly with deionized water and ethanol.
- Perform electrochemical activation through 50 cycles of cyclic voltammetry from -0.2 to +1.5 V in 0.5 M Hâ‚‚SOâ‚„ at 100 mV/s.
Mixed Monolayer Formation:
- Prepare probe solution: 1 µM thiolated DNA probe in trithiol anchoring compound (1:10 ratio) in Tris-EDTA buffer, pH 8.0.
- Incubate electrodes in probe solution for 16 hours at 25°C in a humidified chamber.
- Rinse with PBS to remove physically adsorbed probes.
Surface Crosslinking:
- Prepare 10 mM BM(PEG)3 solution in DMSO.
- Transfer electrodes to crosslinking solution for 4 hours at 25°C.
- Rinse with DMSO followed by PBS to remove unreacted crosslinker.
Hydrophobic Passivation:
- Incubate electrodes in 1 mM hexanethiol solution in ethanol for 1 hour.
- Rinse thoroughly with ethanol and PBS.
Quality Control Assessment:
- Characterize monolayer integrity via electrochemical impedance spectroscopy in 5 mM Fe(CN)₆³â»/â´â».
- Accept sensors with charge transfer resistance (Rct) < 200 Ω for subsequent use.
Detection Protocol for EML4-ALK Fusion Gene
Hybridization and Detection:
- Prepare sample solution containing target EML4-ALK RNA sequence.
- Introduce sample to sensor surface using programmable syringe pump at controlled flow rate of 50 µL/min [54].
- Allow hybridization for 15 minutes at 37°C.
- Perform square wave voltammetry from -0.4 to -0.1 V with amplitude 25 mV, frequency 15 Hz.
- Measure current change relative to baseline; quantify fusion gene concentration from calibration curve.
Calibration and Validation Protocol
Long-Term Stability Assessment:
- Perform daily measurements of standardized positive control (synthetic fusion gene target at 1 nM) over 30-day period.
- Store sensors in PBS at 4°C between measurements.
- Calculate coefficient of variation (CV) for daily measurements; acceptable performance: CV < 15%.
- Monitor signal degradation rate; perform recalibration if signal decrease > 20% from baseline.
Reproducibility Validation:
- Fabricate three independent sensor batches (n=10 per batch).
- Test each sensor with identical sample containing 100 pM target fusion gene.
- Calculate inter-batch and intra-batch CV; acceptable performance: CV < 20%.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Sensor Development
| Item | Function/Application | Example Specifications |
|---|---|---|
| Trithiol Anchoring Compounds | Enhanced monolayer stability via multidentate binding [53] | THIOTRIS; >95% purity; soluble in aqueous buffer |
| BM(PEG)3 Crosslinker | Post-deposition monolayer stabilization [53] | 10 mM solution in DMSO; store at -20°C |
| Hydrophobic Passivation Thiols | Reduced monolayer solubility in aqueous environments [53] | Hexanethiol; 1 mM in ethanol |
| Programmable Syringe Pump | Precise fluid handling for reproducible fabrication and detection [54] | LSPone; flow rate: 0.5 µL/min to 30 mL/min |
| Zwitterionic Monolayer Components | Anti-biofouling surface modification [53] | Carboxybetaine acrylamide; stable at 4°C |
| Stable Redox Reporters | Alternative to methylene blue for improved stability [53] | Ferrocene derivatives; positive reduction potential |
| Flexible Substrate Materials | Mechanical biocompatibility for wearable formats [57] | PDMS; modulus similar to skin (~100 kPa) |
The convergence of stability-enhancing chemistries, reproducible fabrication methodologies, and biocompatible designs creates a pathway for transforming electrochemical fusion gene sensors from research tools into clinically viable diagnostics. The protocols outlined herein provide a framework for developing sensors capable of reliable, long-term operation in complex biological environments. As these technologies mature, they hold the potential to revolutionize cancer diagnosis through point-of-care detection of oncogenic biomarkers, enabling personalized treatment strategies and improved patient outcomes. Future developments should focus on integrating these stabilization strategies with emerging detection platforms and multiplexing capabilities to address the complex landscape of cancer genomics.
The field of cancer diagnostics is undergoing a paradigm shift, moving from traditional, often qualitative methods toward quantitative, data-driven approaches. This transition is particularly evident in the detection of fusion genes—clinically significant biomarkers formed by the joining of two different genes through chromosomal rearrangements. These genetic alterations serve as vital diagnostic, prognostic, and predictive indicators across numerous hematological malignancies and solid tumors, informing targeted therapy selection and monitoring treatment response [13] [58]. The emergence of electrochemical (EC) biosensing platforms for fusion gene detection represents a technological advancement that generates rich, quantitative data ripe for computational analysis. This application note details protocols and methodologies for effectively integrating data analytics and machine learning (ML) with these advanced biosensors to create robust Clinical Decision Support Systems (CDSS). By bridging this gap, we aim to enhance the analytical performance of diagnostic tools and translate complex data into clinically actionable insights, ultimately supporting researchers and drug development professionals in the precision oncology landscape.
Quantitative Performance of Electrochemical Biosensing Platforms
Electroanalytical technologies offer a promising alternative to traditional detection techniques like sequencing and FISH, providing affordable, versatile, and rapid detection without compromising specificity, sensitivity, or accuracy [13]. The performance of these platforms can be quantified against established benchmarks. The following table summarizes key analytical performance metrics from recent studies on EC-based fusion gene detection, providing a baseline for evaluating the impact of subsequent data analytics.
Table 1: Performance Metrics of Electrochemical Biosensors for Fusion Gene Detection
| Target Fusion Gene | Detection Technique | Linear Detection Range | Limit of Detection (LOD) | Reported Sensitivity | Reported Specificity | Clinical/Research Application |
|---|---|---|---|---|---|---|
| BCR-ABL1 | Differential Pulse Voltammetry | 0.1 fM - 10 nM | 0.05 fM | 98.5% | 99.2% | CML Monitoring [58] |
| EML4-ALK | Electrochemical Impedance Spectroscopy | 1 fM - 100 pM | 0.5 fM | 97.0% | 98.8% | NSCLC Targeted Therapy [7] |
| TMPRSS2-ERG | Square Wave Voltammetry | 0.01 pM - 1 nM | 0.01 pM | 99.0% | 98.5% | Prostate Cancer Diagnosis [13] |
| General Fusion Gene Profile | Amperometry | 0.1 pM - 100 pM | 0.1 pM | >95% | >95% | Multi-Gene Panels [7] |
The integration of nanomaterials has been pivotal in achieving these performance characteristics. Nanoparticles (NPs) enhance biosensor performance by improving signal generation and amplification, thereby increasing sensitivity [7]. However, it is critical to note that the use of certain nanomaterials, such as cadmium-based quantum dots, introduces toxicity and biocompatibility concerns that must be thoroughly evaluated for clinical translation [7].
Integrated Experimental Protocol: From Assay to Analysis
This section provides a detailed, end-to-end protocol for executing an electrochemical detection assay and preparing the resulting data for computational analysis.
Protocol: Electrochemical Detection of Fusion Genes with Integrated Data Capture
Principle: This protocol describes the detection of a specific fusion gene (e.g., BCR-ABL1) in extracted RNA samples using a nanoparticle-enhanced electrochemical DNA biosensor. The assay is based on the hybridization of target gene sequences to specific probes immobilized on a screen-printed gold electrode, with signal amplification provided by silver nanoparticles (AgNPs) tagged with report sequences.
I. Materials and Reagent Setup (Pre-Assay)
- Biosensor Chips: Screen-printed gold electrode arrays.
- Capture Probes: Thiol-modified single-stranded DNA (ssDNA) sequences complementary to a conserved region of the target fusion gene (e.g., BCR-ABL1 b2a2 variant). Resuspend in TE buffer to a stock concentration of 100 µM.
- Signal Reporters: AgNPs functionalized with report ssDNA sequences.
- Hybridization Buffer: 6X SSC buffer with 0.1% SDS.
- Washing Buffer: 0.1X SSC buffer.
- Blocking Solution: 1 mM 6-Mercapto-1-hexanol (MCH) in ethanol.
- Sample: Purified RNA from patient samples or cell lines. Include positive controls (synthetic target) and negative controls (non-fusion RNA).
II. Functionalization of the Electrode Surface
- Probe Immobilization: Pipette 2 µL of the 1 µM thiolated capture probe solution onto the working electrode surface. Incubate in a humidified chamber for 60 minutes at room temperature.
- Washing: Rinse the electrode thoroughly with deionized water to remove unbound capture probes.
- Surface Blocking: Incubate the electrode with 5 µL of MCH blocking solution for 30 minutes to passivate uncoated gold surfaces and minimize non-specific binding.
- Final Rinse: Rinse again with deionized water and air dry.
III. Target Hybridization and Signal Amplification
- Sample Denaturation: Denature the RNA sample (or synthetic target) at 95°C for 5 minutes and immediately place on ice.
- Hybridization: Apply 10 µL of the denatured sample to the functionalized electrode and incubate at 37°C for 45 minutes in a humidified chamber.
- Washing: Gently wash the electrode with washing buffer to remove unhybridized material.
- Signal Probe Binding: Apply 10 µL of the AgNP-DNA report probe solution to the electrode. Incubate at 37°C for 30 minutes.
- Final Washing: Perform a stringent wash with washing buffer followed by deionized water.
IV. Electrochemical Measurement and Data Export
- Instrument Setup: Connect the biosensor to a potentiostat. Place the electrode in an electrochemical cell containing a suitable electrolyte (e.g., 0.1 M KCl).
- Signal Development: Immerse the electrode in a silver enhancement solution for 90 seconds to catalytically deposit silver onto the AgNPs.
- Quantitative Measurement: Perform Differential Pulse Voltammetry (DPV) with the following parameters:
- Potential range: -0.2 V to +0.5 V (vs. Ag/AgCl reference)
- Pulse amplitude: 50 mV
- Pulse width: 50 ms
- Scan rate: 20 mV/s
- Data Capture: Record the current (µA) at the characteristic stripping potential of silver (approximately +0.25 V). Export the full voltammogram (Potential vs. Current) and the peak current value as a
.csvfile for subsequent analysis. Ensure metadata (e.g., Sample ID, Assay Date, Electrode Lot) is included.
Workflow Visualization: From Sample to Clinical Insight
The following diagram illustrates the integrated experimental and computational workflow described in this protocol.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of this integrated approach relies on a suite of specialized reagents and computational tools. The following table catalogs the key components and their functions.
Table 2: Research Reagent Solutions for Integrated EC-ML Workflows
| Item Name | Function/Application | Critical Specifications & Notes |
|---|---|---|
| Screen-Printed Electrode (SPE) Array | Platform for probe immobilization and electrochemical transduction. | Gold working electrode preferred. Enables high-throughput, disposable use. |
| Thiol-Modified DNA Capture Probes | Binds specifically to the target fusion gene sequence on the electrode surface. | HPLC-purified. Sequence must be designed against a unique junction of the fusion gene. |
| Silver Nanoparticles (AgNPs) | Signal amplification tag; catalytic deposition enhances electrochemical current. | ~20 nm diameter, functionalized with report DNA. Superior signal-to-noise vs. organic labels. |
| Potentiostat/Galvanostat | Instrument for applying potential and measuring current in electrochemical assays. | Requires software capable of DPV, EIS, and amperometry. Digital data export is essential. |
| Clinical RNA Sample Kit | Isolation and purification of high-quality RNA from patient samples (blood, tissue). | Must yield RNA with high purity (A260/A280 >1.8) and integrity (RIN >7) for reliable results. |
| Python/R with scikit-learn/XAI Libraries | Open-source programming environments for building ML models and explanation tools. | Key libraries: SHAP, LIME, Grad-CAM for model interpretability [59]. |
Integrating Machine Learning for Enhanced Diagnostic Insight
The quantitative data generated by electrochemical biosensors, particularly when configured in multi-analyte arrays, creates a complex dataset ideal for machine learning analysis.
Data Preprocessing and Feature Engineering
Prior to model development, raw voltammetric data must be curated. This involves:
- Baseline Correction: Using algorithms (e.g., asymmetric least squares) to remove background current.
- Peak Alignment & Normalization: Aligning peaks across multiple runs and normalizing current signals to an internal standard.
- Feature Extraction: Deriving features such as peak potential, peak current, peak area, full width at half maximum (FWHM), and shape descriptors from each voltammogram. For multi-sensor arrays, the feature vector will include signals from all channels.
Model Training and Validation for Clinical Decision Support
Supervised learning models can be trained on these feature vectors to perform tasks critical for clinical decision support:
- Classification: Distinguishing between different fusion gene variants (e.g., BCR-ABL1 b2a2 vs. b3a2) or between positive and negative samples.
- Regression: Predicting the concentration of the target fusion gene transcript, which is crucial for monitoring minimal residual disease [13] [60].
- Anomaly Detection: Identifying novel or rare fusion events that deviate from known patterns, potentially flagging them for further investigation.
The implementation of Explainable AI (XAI) is non-negotiable in a clinical context. Model-agnostic techniques like SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) are essential to clarify which features in the voltammetric data most influenced a model's prediction [59]. This transparency helps build trust with clinicians and researchers, allowing them to verify the model's reasoning against clinical knowledge.
Visualizing the Clinical Decision Support Logic
The role of ML and XAI in transforming raw sensor data into a clinical decision is summarized in the following logic pathway.
The integration of data analytics and machine learning with electrochemical biosensing platforms creates a powerful synergy that significantly advances clinical decision support for cancer diagnostics. This combination not only improves the raw sensitivity and specificity of the detection assay itself but, more importantly, unlocks the ability to generate nuanced, predictive, and explainable insights from complex biomarker data. For researchers and drug development professionals, these integrated protocols provide a framework for developing more robust companion diagnostics, identifying patient subgroups for targeted therapies, and monitoring treatment efficacy with unprecedented precision. As the field progresses, the focus must remain on rigorous clinical validation, addressing algorithmic bias to ensure equitable care, and seamless integration of these intelligent systems into clinical workflows to truly bridge the gap between data and decisive action in precision oncology.
Benchmarking Performance: Electrochemical Sensors vs. FISH, PCR, and NGS
The evolution of cancer diagnostics has shifted toward methods that enable earlier and more precise detection. Among these, electrochemical biosensors for detecting cancer-specific fusion genes represent a significant advancement, offering a powerful tool for researchers and clinicians. These biosensors are designed to identify characteristic genetic translocations, such as the BCR/ABL gene in chronic myeloid leukemia (CML) or the PML/RARα gene in acute promyelocytic leukemia (APL), with high specificity and sensitivity [28]. This document provides a detailed comparative analysis of key diagnostic metrics—sensitivity, specificity, and turnaround time—across several cancer detection technologies. It further outlines standardized experimental protocols for developing and validating electrochemical biosensors, serving as a technical guide for scientists and drug development professionals engaged in oncological research.
Comparative Performance of Cancer Diagnostic Modalities
The performance of different cancer detection technologies varies significantly based on their underlying mechanisms. The following table summarizes the reported performance metrics for several diagnostic approaches, including emerging liquid biopsy techniques and established electrochemical biosensors.
Table 1: Comparative Diagnostic Metrics of Cancer Detection Technologies
| Technology / Test Name | Target / Principle | Reported Sensitivity | Reported Specificity | Turnaround Time & Key Features |
|---|---|---|---|---|
| Electrochemical DNA Biosensors (Research Stage) | Detection of fusion genes (e.g., PML/RARα, BCR/ABL) via hybridization and electrochemical signal [28]. | High sensitivity reported in preclinical studies; capable of detecting low-abundance targets [28]. | High specificity reported; minimizes false positives from sequence-specific hybridization [28]. | Hours; Advantages: Low reagent cost, simple operation, minimal instrumentation, high potential for point-of-care use [28]. |
| Galleri MCED Test | Targeted methylation sequencing of cell-free DNA (cfDNA) for >50 cancer types [61]. | 51.5% (all cancers, all stages); 76.3% (12 high-mortality cancers) [61]. | 99.6% (False positive rate of 0.4%) [61]. | Days to weeks; Requires centralized lab; Features: Provides Cancer Signal Origin (CSO) prediction with 93.4% accuracy [61]. |
| Carcimun Test | Detection of conformational changes in plasma proteins via optical extinction [62] [63]. | 90.6% [62] [63]. | 98.2% [62] [63]. | Rapid (based on protocol); Protocol involves simple plasma preparation and spectrophotometric measurement [63]. |
| PanSeer Test | Methylation-based cfDNA assay for stomach, esophageal, colorectal, lung, or liver cancer [64]. | 95% in asymptomatic patients diagnosed within 4 years [64]. | 96% [64]. | Not specified; Notable for demonstrating potential for early detection years before conventional diagnosis [64]. |
| Other MCED (ScienceDirect Study) | cfDNA bisulfite sequencing for >100,000 methylation regions [65]. | 43.9% (all cancers); 67.3% (12 pre-specified cancers, Stages I-III) [65]. | 99.3% [65]. | Implies complex, longer process; Performance varies significantly with cancer stage [65]. |
Experimental Protocol: Electrochemical Detection of Fusion Genes
This protocol details the steps for developing an electrochemical biosensor for the detection of leukemia-related fusion genes, such as PML/RARα.
Principle
The biosensor operates by immobilizing a single-stranded DNA (ssDNA) probe sequence complementary to the target fusion gene on a nanomaterial-enhanced electrode surface. Upon hybridization with the target DNA, a change in the electrochemical properties at the electrode interface occurs, which is measured using techniques like Differential Pulse Voltammetry (DPV). The signal can be further amplified using electroactive indicators (e.g., Methylene Blue) or enzyme-based amplification systems [28].
Materials and Equipment
Table 2: Research Reagent Solutions and Essential Materials
| Item Name | Function / Description |
|---|---|
| Single-Stranded DNA (ssDNA) Probe | The biorecognition element; designed to be complementary to a unique sequence of the target fusion gene (e.g., PML/RARα) [28]. |
| Nanomaterial-enhanced Working Electrode | The transduction platform. Common materials include Gold Nanoparticles (AuNPs), screen-printed carbon electrodes, or graphene. Nanomaterials increase surface area and electrocatalytic activity, enhancing sensitivity [28]. |
| Electrochemical Cell (3-electrode system) | Consists of a Working Electrode, a Reference Electrode (e.g., Ag/AgCl), and a Counter Electrode (e.g., Platinum wire) for controlled electrochemical measurements [28]. |
| Potentiostat | The instrument used to apply potential and measure the resulting current [28]. |
| Methylene Blue (MB) | An electroactive indicator that binds preferentially to double-stranded DNA (hybridized probe), providing an amplified electrochemical signal [28]. |
| Buffer Solutions (e.g., PBS, TE) | For sample dilution, washing, and maintaining a stable pH and ionic strength during hybridization and measurement [28]. |
Step-by-Step Procedure
Electrode Functionalization:
- Clean the working electrode (e.g., gold or glassy carbon) according to standard protocols (e.g., polishing, electrochemical cleaning).
- Immobilize the ssDNA capture probes onto the electrode surface. This can be achieved via covalent bonding (e.g., thiol-gold chemistry for AuNPs), physical adsorption, or using conducting polymers [28].
Hybridization Assay:
- Apply the prepared sample (containing denatured, single-stranded target DNA) to the functionalized electrode surface.
- Incubate under optimized conditions (specific temperature and time, e.g., 37°C for 30 minutes) to allow for hybridization between the target DNA and the immobilized probe.
- Wash the electrode thoroughly with an appropriate buffer (e.g., PBS with mild detergent) to remove any non-specifically bound DNA or contaminants.
Electrochemical Measurement:
- If using an indicator, incubate the electrode with a solution of Methylene Blue.
- Place the electrode into the electrochemical cell containing a suitable electrolyte solution.
- Perform Differential Pulse Voltammetry (DPV) measurements. The parameters may include a potential range from -0.5 V to -0.1 V (vs. Ag/AgCl reference), a step potential of 5 mV, and a modulation amplitude of 50 mV.
- Record the reduction peak current of Methylene Blue, which will decrease upon successful hybridization due to the hindrance of electron transfer [28].
Data Analysis:
- The change in peak current (ΔI) is proportional to the concentration of the target DNA. A standard curve should be established using known concentrations of synthetic target DNA.
- The unknown concentration of target in a sample can be interpolated from this standard curve.
The workflow and the factors influencing key diagnostic metrics are summarized in the following diagrams.
Diagram 1: Experimental Workflow for Electrochemical DNA Biosensing
Diagram 2: Key Factors Influencing Diagnostic Metrics
The data presented in Table 1 highlights a clear trade-space in diagnostic technology. While advanced MCED tests like Galleri offer a broad cancer screening capability with very high specificity, they are complex, likely have longer turnaround times, and exhibit more variable sensitivity, particularly for early-stage cancers [61] [65]. In contrast, electrochemical biosensors, as detailed in the protocol, are designed for a specific, singular diagnostic question—the presence of a particular fusion gene. This focus allows them to achieve high sensitivity and specificity while offering a dramatically faster and simpler analytical process, which is critical for clinical decision-making and minimal residual disease monitoring [28].
The high specificity of these biosensors stems from the fundamental principle of complementary base pairing during DNA hybridization [28]. Their exceptional sensitivity is achieved through the synergistic combination of specific biorecognition elements and the enhanced signal transduction provided by nanomaterials like gold nanoparticles and graphene [28]. Furthermore, the simplified workflow and use of portable potentiometers contribute to a short turnaround time, underscoring their significant potential for point-of-care testing environments [28]. For researchers, this technology provides a robust, cost-effective, and highly specific tool for validating the presence of genetic biomarkers in experimental models, accelerating the pipeline from basic research to clinical application in precision oncology.
The BCR-ABL fusion gene, generated by the Philadelphia chromosome translocation t(9;22), is a well-established molecular driver of several leukemias. It is a defining characteristic of Chronic Myeloid Leukemia (CML) and also present in a subset of Acute Lymphoblastic Leukemia (ALL) [66] [67]. This aberrant gene encodes a constitutively active tyrosine kinase protein that promotes uncontrolled cellular proliferation and suppresses apoptosis, fundamentally driving leukemogenesis [68] [67]. Its detection is not merely diagnostic but is critical for risk stratification, selection of targeted therapy (Tyrosine Kinase Inhibitors or TKIs), and meticulous monitoring of treatment response [13] [66]. While traditional molecular techniques like reverse transcriptase polymerase chain reaction (RT-PCR) and next-generation sequencing (NGS) are standard, the field is increasingly moving towards innovative electrochemical (EC) biosensors. These platforms offer a promising alternative for detecting fusion genes, providing rapid, cost-effective, and highly sensitive analysis without compromising accuracy, which is crucial for advancing personalized medicine in oncology [13] [69] [70].
Clinical and Molecular Background
Disease Context and Pathogenesis
The formation of the BCR-ABL fusion gene is a cornerstone event in the pathogenesis of CML. This genetic aberration occurs when pieces of chromosomes 9 and 22 break off and swap places, creating the shortened chromosome 22 known as the Philadelphia (Ph) chromosome [67]. The product of this gene is an oncogenic fusion protein with dysregulated tyrosine kinase activity, perpetually signaling cells to divide [68]. The World Health Organisation (WHO) has reclassified CML as a biphasic disease (chronic phase and blast phase), moving away from the traditional triphasic model that included an accelerated phase, a shift that impacts prognostic understanding and therapeutic strategies [66].
BCR-ABL Transcript Variants
The breakpoints within the BCR gene can occur in different regions, leading to distinct transcript variants and fusion proteins with slightly different molecular weights and clinical implications. The major breakpoint cluster region (M-BCR) is most common in CML, producing a p210 protein, while breaks in the minor region (m-bcr) produce a p190 protein more often associated with ALL [67].
Table 1: Common BCR-ABL Fusion Transcript Variants and Their Characteristics
| Transcript Variant | Fusion Protein | Primary Disease Association | Prevalence Notes |
|---|---|---|---|
| b3a2 | p210 | Chronic Myeloid Leukemia (CML) | Most prevalent variant in several populations [67] |
| b2a2 | p210 | Chronic Myeloid Leukemia (CML) | Common variant; some studies suggest potential differences in TKI sensitivity [67] |
| e1a2 | p190 | Acute Lymphoblastic Leukemia (ALL) / CML (rare) | Associated with monocytosis in some studies [67] |
Accurate identification of the specific variant is essential as it can influence disease monitoring and potentially even treatment response, with some research indicating that the b2a2 transcript may exhibit different sensitivity to TKIs like imatinib compared to b3a2 [67].
Conventional Detection Methodologies
The diagnosis and monitoring of CML rely on a multi-technique approach to detect the BCR-ABL fusion gene. The 2025 European LeukemiaNet (ELN) recommendations continue to advocate for morphology and chromosome banding analysis (CBA) on bone marrow at diagnosis for disease staging and detection of additional chromosomal abnormalities. Concurrently, RT-PCR on peripheral blood or bone marrow is recommended to precisely identify the BCR-ABL transcript type for baseline assessment and future monitoring [66].
Table 2: Standard Techniques for BCR-ABL Fusion Gene Detection
| Method | Target | Key Advantages | Key Limitations |
|---|---|---|---|
| Chromosome Banding Analysis (CBA) | Entire genome/Chromosomes | Unbiased, detects variant translocations and additional chromosomal abnormalities [71] [66] | Requires live, culturable cells; low resolution and sensitivity; complex procedures [71] |
| Fluorescent In Situ Hybridization (FISH) | DNA sequences (BCR/ABL) | High sensitivity; short turnaround time [71] | Targeted approach; cannot screen for numerous fusions simultaneously [71] |
| Reverse Transcription PCR (RT-PCR) | RNA (Fusion transcript) | High sensitivity; short turnaround time; quantitative capabilities for monitoring [71] [66] | Targeted; cannot screen for numerous fusions; limited if rare transcripts not recognized by commercial kits [71] [66] |
| RNA Sequencing (RNA-seq) | RNA (Transcriptome) | Comprehensive, can detect thousands of known and novel fusions simultaneously [71] | High cost; cannot detect IGH-related rearrangements that don't produce stable RNA [71] |
| Targeted Next-Generation Sequencing (tNGS) | DNA/RNA | Can simultaneously detect gene fusions and other mutations from a single sample [71] | Complex data analysis; higher cost than PCR or FISH |
A significant innovation in conventional testing is the use of targeted NGS on DNA to identify gene fusions. This method involves designing panels that cover intronic regions of genes frequently involved in fusions, such as ABL1 and BCR. When a chromosomal rearrangement occurs, the breakpoints can be captured by probes and sequenced, revealing the fusion partners. This approach allows for the concurrent detection of gene fusions and other mutations, reducing sample requirements and streamlining laboratory workflows [71].
Electrochemical Biosensors for Fusion Gene Detection
Principles and Advantages
Electrochemical biosensors represent a revolutionary approach in molecular diagnostics. These devices integrate a biological recognition element (e.g., a DNA probe) with an electrode transducer that converts a specific biological binding event into a quantifiable electrical signal [69] [70]. For detecting the BCR-ABL fusion gene, a DNA probe complementary to a unique sequence at the fusion junction can be immobilized on the electrode surface. Hybridization with the target DNA or RNA from a patient sample induces a measurable change in electrical properties, such as current (amperometry/voltammetry) or impedance [13] [7].
The compelling advantages of these platforms are their superior sensitivity, potential for high specificity, rapid analysis time, cost-effectiveness, and portability [13] [69] [70]. Unlike traditional methods that are often confined to central laboratories, electrochemical biosensors are highly suited for development as point-of-care (PoC) technologies, which could dramatically expand access to accurate diagnostics in remote or resource-limited settings [69].
Key Experimental Protocol: EC Detection of BCR-ABL
The following protocol outlines a generalized procedure for detecting BCR-ABL fusion gene sequences using an electrochemical biosensor.
1. Biosensor Fabrication and Probe Immobilization
- Electrode Preparation: Clean the working electrode (e.g., gold, glassy carbon) thoroughly via polishing and electrochemical cycling.
- Nanomaterial Functionalization (Optional but recommended): To enhance sensitivity, modify the electrode surface with nanomaterials like graphene oxide, carbon nanotubes, or metal nanoparticles. This increases the active surface area and improves electron transfer [69] [7].
- Probe Immobilization: Covalently attach or adsorb a thiol- or amino-modified single-stranded DNA (ssDNA) probe onto the electrode surface. The probe is designed to be perfectly complementary to the specific "breakpoint" sequence of the target BCR-ABL transcript (e.g., the b3a2 junction). The electrode is then treated with a passivating agent (e.g., 6-mercapto-1-hexanol) to block non-specific binding sites [69].
2. Sample Preparation and Hybridization
- Nucleic Acid Extraction: Isolate total RNA or DNA from a patient's peripheral blood or bone marrow sample using standard commercial kits.
- Target Amplification (If required): For ultra-trace level detection, the target BCR-ABL sequence may be amplified using techniques like PCR. However, a key goal of advanced EC sensors is to achieve direct detection without amplification.
- Hybridization: Incubate the prepared sample with the functionalized biosensor. Under optimized conditions (buffer, temperature, time), the target BCR-ABL sequence will hybridize with the immobilized probe on the electrode surface.
3. Electrochemical Signal Measurement and Readout
- Signal Transduction: After washing away non-specifically bound molecules, the biosensor is placed in an electrochemical cell containing a redox mediator (e.g., [Fe(CN)₆]³â»/â´â»). Techniques like Electrochemical Impedance Spectroscopy (EIS) or Differential Pulse Voltammetry (DPV) are then applied.
- EIS Measurement: The hybridization event insulates the electrode surface, increasing the electrical impedance. The change in charge transfer resistance (Rₑₜ) is directly proportional to the amount of target hybridized [7].
- DPV Measurement: A redox-active molecule (e.g., methylene blue) that preferentially binds to double-stranded DNA can be used. The measured reduction in current peak is correlated to the concentration of the target fusion gene [70].
- Data Analysis: The electrochemical signal (current or impedance) is calibrated against known standards to quantify the level of BCR-ABL in the patient sample.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for BCR-ABL Electrochemical Biosensing
| Reagent/Material | Function/Description | Example Application in Protocol |
|---|---|---|
| DNA Probe (ssDNA) | The recognition element; designed to be complementary to the unique BCR-ABL fusion junction sequence. | Immobilized on the electrode surface to capture the target nucleic acid. |
| Nanomaterials (e.g., Graphene, AuNPs) | Signal amplification; enhance electrode surface area and facilitate electron transfer, boosting sensitivity. | Used to modify the electrode surface prior to probe immobilization [69] [7]. |
| Redox Mediators (e.g., [Fe(CN)₆]³â»/â´â») | Generate electrochemical signal; their behavior changes upon target binding, providing a measurable signal. | Added to the solution for EIS or DPV measurements after hybridization [7]. |
| Passivating Agents (e.g., MCH) | Block non-specific binding; form a monolayer on the electrode to prevent false-positive signals. | Applied after probe immobilization to cover any unreacted surface sites [69]. |
| Hybridization Buffer | Create optimal conditions for specific binding between the probe and target sequence. | The solution used during the incubation of the sample with the biosensor. |
Data Presentation and Analysis
Electrochemical biosensors generate quantitative data that can be effectively used for both qualitative detection and quantitative monitoring of BCR-ABL levels, which is vital for assessing treatment response over time.
Table 4: Representative Electrochemical Signal Data for BCR-ABL Detection
| Target Concentration (pM) | DPV Peak Current (µA) | EIS Charge Transfer Resistance (Rₑₜ, Ω) | Notes / Clinical Correlation |
|---|---|---|---|
| 0 (Blank) | 25.0 | 500 | Baseline / negative control |
| 1 | 23.5 | 1200 | Limit of Detection (LOD) level |
| 10 | 20.1 | 3500 | Low-level positive |
| 100 | 15.2 | 8500 | High-level positive (e.g., at diagnosis) |
| Post-TKI (Theoretical) | 24.1 | 900 | Corresponds to molecular response |
The relationship between the target concentration and the electrochemical signal can be visualized to create a calibration curve. In DPV, the peak current decreases as the amount of target fusion gene hybridized on the electrode increases. Conversely, in EIS, the charge transfer resistance (Rₑₜ) increases with higher target concentration due to greater obstruction of electron transfer. This quantitative output allows for tracking a patient's molecular response to Tyrosine Kinase Inhibitor (TKI) therapy, with the signal parameters approaching baseline levels as the BCR-ABL transcript load decreases [13] [70].
The detection of the BCR-ABL fusion gene remains a non-negotiable pillar in the modern management of CML and Ph+ ALL. While robust conventional techniques like RT-PCR and FISH are the current clinical mainstays, the emerging paradigm of electrochemical biosensing offers a transformative potential. These platforms, especially when enhanced with nanotechnology, promise a future with faster, more sensitive, and more accessible diagnostics [13] [69]. Integrating these biosensors into clinical practice could revolutionize patient monitoring, enabling more frequent testing and quicker therapeutic adjustments. Furthermore, their inherent suitability for point-of-care deployment holds the promise of democratizing precision oncology, ensuring that all patients, regardless of location, have access to the high-quality diagnostic tools essential for optimal outcomes. Continued research and development in this interdisciplinary field are poised to make this future a reality.
Cost-Benefit and Accessibility Analysis for Routine Screening and Point-of-Care Use
The integration of advanced diagnostic technologies into clinical practice necessitates a rigorous evaluation of their economic value and practical accessibility. For novel electrochemical biosensors designed to detect cancer-related fusion genes, this analysis is paramount to guide their translation from research laboratories to routine clinical and point-of-care (POC) settings. These emerging technologies promise significant advancements in early cancer detection, minimal residual disease (MRD) monitoring, and personalized treatment strategies. However, their widespread adoption depends not only on analytical performance but also on a favorable cost-benefit profile and the ability to be deployed accessibly across diverse healthcare environments. This application note provides a structured framework for evaluating the cost-benefit and accessibility of such diagnostic platforms, synthesizing current economic data, detailing standardized experimental protocols for validation, and outlining key implementation considerations for researchers, scientists, and drug development professionals.
A critical step in the evaluation process is benchmarking new technologies against the established cost-effectiveness of current cancer screening and diagnostic methods. The data presented below provide a reference for the economic landscape.
Table 1: Cost-Utility of Selected Cancer Interventions and Screening [72] [73]
| Cancer Type / Category | Median Incremental Cost-Effectiveness Ratio (ICER) per QALY (2014 USD) | Annual Screening Cost (Initial Tests Only) | Key Contextual Notes |
|---|---|---|---|
| Breast Cancer | $25,000 | $8.8 billion | Represents 20.4% of total annual screening cost for five major cancers. |
| Colorectal Cancer | $24,000 | $27.5 billion | Colonoscopy is the primary driver, accounting for 63.6% of total screening costs. |
| Prostate Cancer | $34,000 | $0.7 billion | Cost-effectiveness is frequently questioned; potential for overdiagnosis. |
| Primary Prevention | $23,000 | Not Applicable | Includes strategies like chemoprevention and vaccination. |
| Secondary Prevention | $34,000 | Not Applicable | Predominantly includes population screening programs. |
Table 2: Cost-Benefit Analysis of a Point-of-Care Testing Model [74]
| Parameter | Central Laboratory Testing | Point-of-Care Testing (iSTAT Analyzer) |
|---|---|---|
| Total Wait Time for Results (35 patients) | 526 minutes | 105 minutes (estimated) |
| Cost Components | Technician callback, paramedic overtime, aircraft wait time | Device cost (~$8,000 CAD), disposable cartridges |
| Total Cost Saving with POC | - | $4,220 CAD (over study period) |
| Breakeven Point | - | 101 patients (with aircraft costs) |
Experimental Protocols for Validation
To ensure that new electrochemical biosensors meet the necessary standards for accuracy and reliability, the following validation protocols should be adopted. These are adapted from established molecular diagnostic methods.
Protocol for Comparative Analytical Validation
This protocol is designed to benchmark the performance of a novel electrochemical biosensor against a gold-standard method, such as quantitative PCR (qPCR), using clinically relevant samples.
1. Sample Preparation:
- Collect peripheral blood or bone marrow samples in EDTA-containing tubes from patients and healthy controls under an approved ethical protocol.
- Extract total RNA using a commercial silica-membrane-based kit. Assess RNA purity and concentration using spectrophotometry (e.g., A260/A280 ratio ~2.0).
- Synthesize cDNA using a reverse transcription kit with random hexamers and/or gene-specific primers.
2. Parallel Testing with Reference Method:
- qPCR (Gold Standard): Perform qPCR reactions in triplicate using TaqMan assays specific for the target fusion gene (e.g., BCR::ABL) and a reference gene (e.g., ABL). Calculate the target/reference ratio expressed as an International Scale (IS) percentage [75].
- Electrochemical Biosensor Testing: Apply the same cDNA samples to the electrochemical biosensor platform. The protocol will vary by design but generally involves:
- Immobilization: Functionalize the sensor electrode with capture probes (e.g., single-stranded DNA complementary to a segment of the fusion gene).
- Hybridization: Incubate the electrode with the denatured cDNA sample to allow target-probe hybridization.
- Signal Generation & Detection: Introduce a redox-active reporter (e.g., methylene blue) and apply a voltage sweep. Measure the resulting current, which is proportional to the amount of captured target [76].
3. Data Analysis:
- Use statistical tests (e.g., Wilcoxon signed-rank test) to assess the significance of differences between the two methods.
- Determine correlation using Spearman's rank correlation coefficient.
- Evaluate agreement using Bland-Altman analysis, plotting the difference between the two methods against their average [75].
Protocol for Cost-Benefit Analysis in a Model Workflow
This protocol outlines a model for evaluating the economic impact of implementing a POC biosensor in a specific clinical pathway.
1. Define the Clinical Scenario:
- Select a clear use case, such as "post-treatment monitoring of CML patients for BCR::ABL MRD" or "rapid diagnosis of suspected acute leukemia in an emergency department."
2. Map the Workflow and Identify Cost Drivers:
- Standard Laboratory Workflow: Document all steps from sample collection, transport, central lab processing (including technologist time, reagents, equipment maintenance), and result reporting.
- POC Biosensor Workflow: Document steps performed at the bedside or clinic, including sample preparation, cartridge use, and device operation.
3. Measure and Value Resources:
- Direct Costs: Calculate consumables (sensor cartridges, reagents), equipment (amortized purchase price), and personnel time for both workflows.
- Indirect Costs & Benefits: Quantify time savings (e.g., reduced stabilization time prior to transport [74]), impact on bed occupancy, and cost avoidance from faster clinical decision-making (e.g., earlier discharge or treatment adjustment).
4. Calculate Cost-Benefit Metrics:
- Simple Cost Comparison: Total the costs per test for each workflow.
- Incremental Cost-Effectiveness Ratio (ICER): If health outcomes data are available, calculate the ICER as: (CostPOC - CostLab) / (EffectivenessPOC - EffectivenessLab). Effectiveness can be measured in QALYs or a disease-specific outcome like time to correct diagnosis.
Visualization of Workflows and Relationships
The following diagrams illustrate the core analytical and economic concepts underpinning this analysis.
Diagram: Electrochemical DNA Biosensor Mechanism
Diagram: Comparative Cost-Benefit Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Successful development and validation of electrochemical biosensors for fusion gene detection rely on a suite of specialized reagents and materials.
Table 3: Essential Materials for Electrochemical Fusion Gene Detection
| Item | Function/Brief Explanation | Example/Note |
|---|---|---|
| Gold or Carbon Electrode | The transduction platform. Gold allows for easy thiol-based functionalization of DNA probes; carbon electrodes are often lower cost and offer a wide potential window. | Screen-printed electrodes are popular for disposable POC devices. |
| Thiol- or Amino-Modified DNA Capture Probes | Single-stranded DNA oligonucleotides designed to be complementary to a unique sequence of the target fusion gene. The modification enables covalent attachment to the electrode surface. | Probe design is critical for specificity, especially to avoid cross-hybridization with wild-type sequences. |
| Redox-Active Reporters | Molecules that undergo reversible oxidation/reduction, generating a measurable current. They can be intercalated into the DNA duplex or be tag-specific. | Methylene Blue, Ferrocene derivatives, or metal nanoparticles (e.g., AuNPs [76]). |
| Blocking Agents (e.g., MCH) | Used after probe immobilization to passivate unused electrode surface areas, minimizing non-specific adsorption and reducing background noise. | 6-Mercapto-1-hexanol (MCH) is standard for gold surfaces. |
| Hybridization Buffer | A solution optimized to promote specific and efficient binding between the capture probe and the target cDNA sequence while minimizing non-specific interactions. | Typically contains salts (e.g., NaCl) and buffering agents (e.g., Tris-EDTA). |
| Signal Amplification Systems | Strategies to enhance the detection signal, crucial for detecting low-abundance targets like fusion genes in MRD. | Enzymatic labels (e.g., Horseradish Peroxidase), nanomaterials like graphene/AuNPs [76], or catalytic hairpin assembly. |
| Portable Potentiostat | The electronic instrument that applies the controlled potential to the electrode and measures the resulting current. Miniaturized versions are key for POC applications. | Commercially available handheld or smartphone-interfaced potentiostats. |
The precise detection of gene fusions, a critical class of biomarkers in oncology, is essential for cancer diagnosis, prognosis, and the administration of targeted therapies [41]. While targeted RNA sequencing (RNA-Seq) offers comprehensive and high-throughput detection, its application in routine clinical practice and point-of-care settings is limited by factors including cost, turnaround time, and the need for sophisticated infrastructure [77] [41]. Electrochemical sensors present a promising complementary technology, offering rapid, cost-effective, and portable analysis. This Application Note delineates a synergistic framework that integrates these two methodologies, leveraging the discovery power of RNA-Seq with the rapid validation and quantification capabilities of electrochemical biosensors for enhanced cancer diagnostics. The core of this approach involves using RNA-Seq for initial biomarker discovery and panel design, followed by the deployment of electrochemical sensors for routine monitoring, therapeutic drug monitoring (TDM), and point-of-care testing (POCT).
The integration of targeted RNA sequencing and electrochemical sensing creates a powerful workflow for cancer biomarker analysis. Targeted RNA-Seq serves as the discovery and comprehensive profiling tool, ideal for identifying novel fusions and validating large panels of biomarkers in a clinical laboratory setting. In parallel, electrochemical sensors can be developed based on the sequences identified by RNA-Seq. These sensors are then deployed for rapid, specific, and quantitative detection of known, clinically actionable fusion genes, such as EML4-ALK or FGFR2 fusions, in resource-limited environments [78] [41]. This synergy is further enhanced by emerging technologies, including CRISPR-Cas systems for improved specificity and artificial intelligence (AI) for data analysis and sensor optimization [79] [80].
Table 1: Comparison of Targeted RNA Sequencing and Electrochemical Sensors for Fusion Gene Detection
| Characteristic | Targeted RNA Sequencing | Electrochemical Sensors |
|---|---|---|
| Primary Role | Discovery, comprehensive profiling | Rapid validation, quantitative point-of-care detection |
| Throughput | High (multiplexed) | Low to medium (single-plex or limited multiplex) |
| Sensitivity | High (can detect low-frequency fusions) | Very High (can achieve sub-micromolar limits of detection) [81] |
| Turnaround Time | Hours to days | Minutes to hours |
| Cost per Assay | High | Low (e.g., ~$0.50 per sensor) [80] |
| Infrastructure Needs | Complex (sequencers, bioinformatics) | Simple (portable potentiostats) |
| Key Strengths | Detects known and novel fusions, genome-wide | Rapid, cost-effective, portable, suitable for therapeutic drug monitoring |
Experimental Protocols
Protocol 1: Designing an Electrochemical RNA Sensor for a Known Fusion Gene
This protocol details the development of a homogeneous electrochemical sensor for detecting a specific fusion gene transcript, such as EML4-ALK variant 1.
3.1.1 Principle The assay, inspired by the HELEN-DR system, utilizes a FAM-RNA-MB reporter probe [77]. The RNA sequence in the probe is complementary to the target fusion junction. Upon hybridization, the formed RNA-DNA heteroduplex is recognized and cleaved by RNase H, an endonuclease that specifically degrades the RNA strand in RNA-DNA duplexes [77]. This cleavage releases a FAM-labeled fragment, altering the electrochemical signal measured via differential pulse voltammetry (DPV).
3.1.2 Workflow
3.1.3 Materials and Reagents Table 2: Key Research Reagent Solutions
| Item | Function/Description | Example Vendor |
|---|---|---|
| FAM-RNA-MB Probe | Dual-labeled reporter; RNA sequence complementary to fusion junction, FAM for fluorescence, MB for electrochemistry. | Custom synthesis (e.g., Sangon Biotech [77]) |
| RNase H Enzyme | Non-specific endonuclease; cleaves RNA strand in RNA-DNA heteroduplex, enabling signal amplification. | Beyotime Biotech [77] |
| Screen-Printed Carbon Electrodes (SPCEs) | Disposable, miniaturized working electrodes; ideal for point-of-care testing. | Various suppliers |
| Portable Potentiostat | Instrument for applying potential and measuring current; enables field-deployable electrochemical detection. | Various suppliers |
| Polyvinyl Alcohol (PVA) | Polymer coating; stabilizes DNA/RNA on electrode surface, extending shelf-life. | Sigma-Aldrich [80] |
3.1.4 Procedure
- Probe Design: Design the RNA sequence within the FAM-RNA-MB probe to be perfectly complementary to the unique junctional sequence of the target fusion gene (e.g., EML4-ALK).
- Sample Preparation: Amplify the target region from patient RNA extracts using isothermal amplification methods like Recombinase Polymerase Amplification (RPA) to produce sufficient single-stranded DNA (ssDNA) for detection [77].
- Assay Setup: In a homogeneous solution, mix the FAM-RNA-MB probe with the amplified ssDNA target.
- Hybridization & Cleavage: Incubate the mixture with RNase H. If the target is present, hybridization occurs, triggering RNase H-mediated cleavage of the RNA strand.
- Detection: Transfer the solution to an electrochemical cell with SPCEs. Measure the DPV signal. A significant decrease in the methylene blue redox signal indicates successful cleavage and, therefore, the presence of the target fusion transcript.
Protocol 2: CRISPR-Cas12a-Based Electrochemical Sensor for DNA Fusion Genes
This protocol leverages the collateral cleavage activity of the CRISPR-Cas12a system for highly specific detection of DNA-level fusion events.
3.2.1 Principle The guide RNA (gRNA) is programmed to recognize the specific DNA fusion junction. Upon target binding, the Cas12a enzyme is activated and exhibits nonspecific "collateral" cleavage activity against nearby single-stranded DNA (ssDNA) [80]. An ssDNA molecule tagged with a redox reporter (e.g., methylene blue) is immobilized on a gold electrode. Cas12a's collateral cleavage severs this ssDNA, causing the reporter to diffuse away and resulting in a measurable drop in the electrochemical current.
3.2.2 Workflow
3.2.3 Materials and Reagents
- Cas12a Enzyme: CRISPR-associated enzyme providing sequence-specificity and signal amplification via collateral cleavage.
- Custom gRNA: Designed to span the breakpoint of the DNA fusion gene.
- Thiol-modified ssDNA Reporter: Immobilized on the gold electrode via thiol-gold chemistry; serves as the substrate for collateral cleavage.
- Gold Leaf Electrodes: Inexpensive substrate for ssDNA immobilization [80].
- Polyvinyl Alcohol (PVA): Used to create a stable protective coating over the functionalized electrode, significantly enhancing its shelf-life at elevated temperatures [80].
3.2.4 Procedure
- Electrode Functionalization: Immobilize thiol-modified ssDNA reporters onto the surface of a gold leaf electrode.
- Stabilization (Optional but Recommended): Coat the functionalized electrode with a thin film of PVA and allow it to dry. This "tarp" protects the DNA, enabling long-term storage [80].
- CRISPR Reaction: Pre-incubate the patient DNA sample (which can be pre-amplified) with the Cas12a-gRNA ribonucleoprotein complex.
- Signal Generation: Apply the reaction mixture to the functionalized electrode. If the target is present, activated Cas12a will cleave the ssDNA reporters on the electrode surface.
- Measurement: Use a portable potentiostat to perform DPV. A reduction in current compared to a negative control confirms the detection of the target fusion gene.
Data Analysis and AI Integration
The quantitative data generated by electrochemical sensors are highly amenable to advanced analysis. Machine Learning (ML) and Artificial Intelligence (AI) algorithms can be integrated to overcome challenges such as signal noise and interference in complex biofluids [79].
- Signal Optimization: AI can screen electrode modification materials (e.g., MXenes, carbon nanotubes) and predict their performance, optimizing sensor sensitivity [81] [79].
- Data Interpretation: Algorithms like Support Vector Machines (SVM) or Convolutional Neural Networks (CNNs) can be trained to recognize specific electrochemical signal patterns, distinguishing true positive signals from background noise or non-specific binding events [79]. This is crucial for achieving high diagnostic accuracy in the analysis of clinical samples like serum or saliva.
Concluding Remarks
The confluence of targeted RNA sequencing and electrochemical sensing establishes a robust paradigm for precision oncology. While RNA-Seq remains the unrivaled tool for discovery and comprehensive genomic profiling, electrochemical sensors provide an agile, affordable, and deployable platform for tracking specific, clinically relevant gene fusions. This synergistic relationship promises to accelerate diagnostic workflows, facilitate therapeutic drug monitoring, and ultimately make advanced molecular diagnostics more accessible at the point of care. Future efforts will focus on increasing the multiplexing capacity of electrochemical sensors and further integrating AI-driven analytics for fully automated, diagnostic-grade results.
Conclusion
The integration of electrochemical biosensing with fusion gene analysis represents a paradigm shift with immense potential to reshape cancer diagnostics. This review synthesizes evidence demonstrating that electrochemical genosensors can meet, and in some aspects surpass, the performance of traditional methods like FISH and PCR, particularly in terms of sensitivity, cost, and speed. While challenges in selectivity in complex media, device miniaturization, and robust clinical validation remain, ongoing advancements in nanotechnology, surface chemistry, and data integration are steadily providing solutions. Future directions must focus on large-scale clinical studies to correlate sensor signals with clinical outcomes, the development of standardized, multiplexed panels for key fusion genes, and navigating the regulatory pathway for clinical adoption. The ultimate goal is the realization of affordable, point-of-care devices that enable widespread, early detection of fusion gene-driven cancers, facilitating timely intervention and personalized medicine on a global scale.
References
- 1. Oncogenic gene fusions in cancer: from biology to therapy [https://www.nature.com/articles/s41392-025-02161-7]
- 2. Fusion genes in cancers: Biogenesis, functions, and ... [https://www.sciencedirect.com/science/article/pii/S235230422500025X]
- 3. Clinical characterization and therapeutic targeting of fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988278/]
- 4. KinaseFusionDB: an integrative knowledge of kinase fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12140011/]
- 5. Clinical characterization and therapeutic targeting of fusion ... [https://pubmed.ncbi.nlm.nih.gov/40128124/]
- 6. a next-gen technology in cancer biomarker detection [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr01675d?page=search]
- 7. Electrochemical detection techniques and usage of ... [https://link.springer.com/article/10.1007/s44373-025-00066-2]
- 8. Gene Fusion: Definition, Mechanisms, Types, Consequences and Detection – Genetic Education [https://geneticeducation.co.in/gene-fusion/]
- 9. Discovering and understanding oncogenic gene fusions through data intensive computational approaches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4889949/]
- 10. Chromosomal translocation [https://en.wikipedia.org/wiki/Chromosomal_translocation]
- 11. Gene fusion as an important mechanism to generate new ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9199173/]
- 12. Improved Gene Fusion Detection in Childhood Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8830514/]
- 13. Electrochemical detection of fusion genes [https://www.sciencedirect.com/science/article/abs/pii/S0013468625018298]
- 14. a review advancements and prospects for cancer diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913392/]
- 15. Accurate and efficient detection of gene fusions from RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919457/]
- 16. Advances in electrochemical biosensors for the detection ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1556595/full]
- 17. MXene-based electrochemical sensors for cancer ... [https://pubmed.ncbi.nlm.nih.gov/41219542/]
- 18. Breaking barriers in cancer diagnosis - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra08212e?page=search]
- 19. HER-2-Targeted Electrochemical Sensors for Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024968/]
- 20. a next-gen technology in cancer biomarker detection [https://pubmed.ncbi.nlm.nih.gov/40899154/]
- 21. Development of a miniaturized electrochemical biochip [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1611743/full]
- 22. Functional nucleic acid-based miniaturized homogeneous ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25030401]
- 23. Next Generation Sequencing for Gene Fusion Analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7460167/]
- 24. Fusion Gene Detection [https://help.partek.illumina.com/partek-flow/user-manual/task-menu/variant-analysis/fusion-gene-detection]
- 25. Immobilization of Antibodies by Genetic Fusion to a Fungal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8561437/]
- 26. Hybridization capture vs amplicon sequencing | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/targeted-sequencing-hybridization-capture-or-amplicon-sequencing/]
- 27. Electrochemical detection of fusion genes [https://www.sciencedirect.com/science/article/pii/S0013468625018298]
- 28. Electrochemical Biosensors in the Diagnosis of Acute and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9817807/]
- 29. A Multiplexed Amplicon Approach for Detecting Gene ... [https://www.sciencedirect.com/science/article/pii/S1525157815002573]
- 30. Efficient Determination of PML/RARα Fusion Gene by the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8144022/]
- 31. Leveraging electrochemical sensors to improve efficiency of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10989266/]
- 32. Revolutionary advances in nanomaterials-based ... [https://www.sciencedirect.com/science/article/pii/S2666831925001110]
- 33. DNA Diagnostics: Nanotechnology-enhanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2876983/]
- 34. Recent Development of Graphene Based Electrochemical ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2021.735668/full]
- 35. Carbon Nanotube Amplification Strategies for Highly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2482602/]
- 36. Carbon Nanotubes-Based Assays for Cancer Detection ... [https://www.mdpi.com/1999-4923/14/4/781]
- 37. Nanomaterial-enhanced electrochemical immunosensor ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25025378]
- 38. Gene fusion detection in long-read transcriptome sequencing ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11866-6]
- 39. Artificial intelligence-assisted electrochemical sensors for ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d4dd00318g]
- 40. Electrochemical Duplex Detection of E2 and E6 Genes of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898155/]
- 41. Challenges and prospects in utilizing technologies for ... [https://link.springer.com/article/10.1007/s44258-024-00033-3]
- 42. Automated sample-to-answer system for rapid and ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400523000977]
- 43. Development and application of a whole transcriptome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063385/]
- 44. Anti-Biofouling Strategies for Long-Term Continuous Use ... [https://www.mdpi.com/2227-9040/8/3/66]
- 45. Mitigating the Effects of Electrode Biofouling-Induced ... [https://pubmed.ncbi.nlm.nih.gov/32298105/]
- 46. Dual-action prevention of adherent and non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439328/]
- 47. MRM3 quantitation for highest selectivity in complex matrices [https://sciex.com/tech-notes/technology/mrm3-quantitation-for-highest-selectivity-in-complex-matrices]
- 48. Multiplexed Cancer Biomarker Detection Using Chip ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5070463/]
- 49. Ultrasensitive electrochemical detection of BCR/ABL fusion ... [https://www.sciencedirect.com/science/article/abs/pii/S1388248113003081]
- 50. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 51. Clinical research 5: Quantitative data collection and analysis [https://www.sciencedirect.com/science/article/pii/S0964339705000406]
- 52. Gene fusion: Mechanisms, detection, and applications [https://www.abcam.com/en-us/knowledge-center/dna-and-rna/gene-fusion-mechanisms-detection-and-applications]
- 53. The challenge of long - term for nucleic acid-based... stability [https://pmc.ncbi.nlm.nih.gov/articles/PMC9455832/]
- 54. Continuous Biosensing: Exploring Long - Term Sensor Stability [https://amf.ch/new-research-in-continuous-biosensing-long-term-stability/]
- 55. In Vivo Chemical Sensors: Role of Biocompatibility on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6773264/]
- 56. AI-optimized electrochemical aptasensors for stable, ... [https://www.sciencedirect.com/science/article/pii/S2405844024173690]
- 57. Biocompatible and Long-Term Monitoring Strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10054135/]
- 58. Electrochemical detection of fusion genes: Advancing ... [https://is.muni.cz/publication/2525822/en?lang=en]
- 59. Explainable AI in Clinical Decision Support Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 60. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 61. Galleri Test Sensitivity & Specificity | Galleri® for HCPs [https://www.galleri.com/hcp/galleri-test-performance]
- 62. Evaluation of an innovative multi-cancer early detection test [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1520869/full]
- 63. Evaluation of an innovative multi-cancer early detection test [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922694/]
- 64. Non-invasive early detection of cancer four years before ... [https://www.nature.com/articles/s41467-020-17316-z]
- 65. Sensitive and specific multi-cancer detection ... [https://www.sciencedirect.com/science/article/pii/S0923753420360580]
- 66. 2025 European LeukemiaNet recommendations for the ... [https://www.nature.com/articles/s41375-025-02664-w]
- 67. BCR-ABL fusion genes and laboratory findings in patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5771363/]
- 68. BCR-ABL: The molecular mastermind behind chronic ... [https://www.sciencedirect.com/science/article/pii/S1359610125000474]
- 69. Nanoengineered electrochemical biosensors: a next-gen ... [https://pubs.rsc.org/en/content/articlelanding/2025/nr/d5nr01675d]
- 70. a review advancements and prospects for cancer diagnosis [https://pubmed.ncbi.nlm.nih.gov/40079211/]
- 71. Detection of leukemia gene fusions on DNA-level through ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0332407]
- 72. Cost-Utility Analysis of Cancer Prevention, Treatment, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5846573/]
- 73. What Is the Value in Cost and Lives Saved of Cancer ... [https://ascopost.com/issues/may-25-2025/what-is-the-value-in-cost-and-lives-saved-of-cancer-screening-and-prevention/]
- 74. : Cost of benefit - point - of blood gas care vs. laboratory... analysis [https://pubmed.ncbi.nlm.nih.gov/14694897/]
- 75. æ•°å—PCR与实时è§å…‰å®šé‡PCR检测慢性髓性白血病患者BCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC10753264/]
- 76. 超çµæ•ç”µåŒ–å¦DNAç”Ÿç‰©ä¼ æ„Ÿå™¨å¯ç”¨äºŽæ—©æœŸç–¾ç—…æ£€æµ‹å’Œè¯Šæ– ... [https://www.vbdata.cn/newsDetail/12ac5ecc7a3211ea9aa400163e0cb09b]
- 77. An electrochemical, fluorescent, and colorimetric triple ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400524004520]
- 78. RNA Sensor Platform for Targeting Cancer Fusion Genes and ... [http://skysong.technologypublisher.com/tech/RNA_Sensor_Platform_for_Targeting_Cancer_Fusion_Genes_and_Transcripts]
- 79. AI-Empowered Electrochemical Sensors for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384469/]
- 80. MIT engineers develop electrochemical sensors for cheap ... [https://news.mit.edu/2025/mit-engineers-develop-electrochemical-sensors-cheap-disposable-diagnostics-0701]
- 81. Recent Advances in Electrochemical Sensors for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563010/]